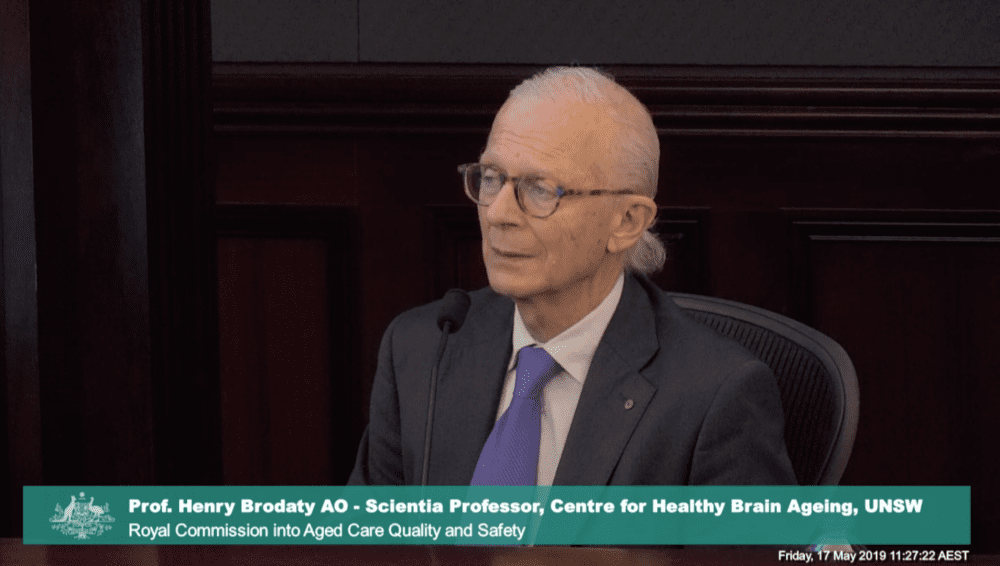
One of the nation’s leading dementia experts and a widely respected dementia advocate addressed the royal commission on Friday, explaining the challenges they see in the aged care sector and dementia care, and the solutions they propose.
Professor Henry Brodaty, Scientia Professor at the Centre for Healthy Brain Ageing at the University of New South Wales, said residents in aged care are “very lonely”.
One researcher found that the median number of relationships a resident in a nursing home had was one – which means 50 per cent had no relationships at all in the nursing home.
“Staff are busy doing their tasks and they have their tasks, there are a lot of tasks to do,” Prof Brodaty said.
“People do need help with feeding, they do need help with cleaning, and are often incontinent, need to be cleaned up and so on, but they don’t focus on the person. No one actually sits down and talks to the person and spends some time with them.”
Prof Brodaty said person centered care reduced agitation for residents living with dementia. He said some providers say they provide person-centered care but in reality, they are not, although the provision of person-centered care is “getting a little bit better”.
Prof Brodaty said nurses skills, such as creative talents, could be better utilised in nursing homes.
“One of my colleagues suggested we should actually be working with the nurses to find out what they like doing and so that we can employ their talents more usefully,” he said.
GPs, aged care providers and family should all be accountable for prescribing psychotropic medications, Prof Brodaty said.
The current practice requires that GPs obtain consent from the family of a resident living with dementia before prescribing a psychotropic medication, although he said he was not aware of any cases when a GP was prosecuted for not going gaining that consent.
“So if the doctor is prescribing, the doctor needs to be certain that consent has been provided,” he said.
If the family isn’t there, the doctor will often ask a nurse to ask the family for their consent when they next visit.
“It’s often difficult for the doctor, particularly in a nursing home where the proxy is not available and so the doctor may and often does delegate that to the nursing staff, saying, “Next time, this person’s spouse or child comes in, could you ask them to sign the consent for that.”
Prof Brodaty said it would be “advisable” for the person who is actually giving out the medication to have an “easy way for them to say that this documentation had been provided”.
Aged care facilities themselves and family also have some responsibility, Prof Brodaty said.
Prof Brodaty said his research in a small number of nursing homes found that only 6.5 per cent of those prescribed psychotropics had received written consent and 6.5 had received verbal consent – so 87 per cent had received no consent. He said he has been advised the rates of consent would be even lower hospitals.
The family also has a responsibility to question why the medication was prescribed, he said.
“Often families just leave it to the doctors or nurses to say ‘well, so-and-so needs this’ rather than questioning why,” Prof Brodaty said. “It’s a bit simplistic to put it all on the doctor, although I think the doctor is the primary person in this chain.”
Prof Brodaty said aged care providers need to balance quality of life with duty of care.
He told the hearing about a resident with Parkinson’s disease who enjoyed walking, and sometimes even walked outside the home, and onto the road.
“Because of his Parkinson’s disease, he would sometimes freeze and if he’s in the middle of the road that’s obviously dangerous. So the nursing home said he’s not allowed to go out, and he became quite agitated,” Prof Brodaty said.
The resident’s wife said, “I’m very happy for him to walk and to take that risk because his quality of life is more important than his safety”.
“This is a tension,” Prof Brodaty said.
The nursing home said, “We respect that but it’s our reputation. If he gets hit by a car, we bear the responsibility. It will be all over the… media and it’s very bad for the nursing home”, and they refused to allow the man to leave the nursing home.
“I understand both points of view,” Prof Brodaty said.
“The nursing home does have what they call a duty of care and responsibility, but there’s this… tension between cotton wool, safety, autonomy and independence.”
“It’s one of these wicked problems that we have in looking after people in nursing homes,” he said.
He suggested advanced care directives could be a way to resolve this tension.
Prof Brodaty said residents, not profit, must be the operator’s top priority to deliver person-centred care.
“Management needs to embrace this as a philosophy for their nursing home, or most commonly now chains of nursing homes, and so that needs to come from the top management, but also the director of nursing needs to also say this is our philosophy, that really the person is our first priority.
“It’s not about profit. I’m not saying that all nursing homes work just on profit.
“But it’s trying to make their life as good as possible, the people living there, and for most people going to nursing homes this is their home and this is their final home.
Kate Swaffer was the final speaker on Friday, the last day of the Sydney hearings.
Ms Swaffer was diagnosed with a rare form of young onset dementia at the age of 49. She is the chair and chief executive officer of Dementia Alliance International, and organisation set up five years ago by eight people with dementia from three different countries.
Dementia Alliance International provides peer-to-peer support on an almost daily basis for members around the world, and now has thousands of members representing currently 49 countries. The organisation provides monthly educational webinars for people with dementia, their families and the wider community, including the dementia sector, and has a range of free, online services for people with dementia.
Ms Swaffer said when she was diagnosed she was told to give up work, give up studying, get her affairs in order, and prepare to live in a nursing home.
But she told the royal commission people diagnosed with dementia should be supported to stay at work, and accommodated for any changes to their abilities. She said counselling would also be helpful. The goal should be for people living with dementia to be helped to live independently for longer.
Ms Swaffer said the aged care system has moved to a situation where aged care residents and people living with dementia are “incarcerated”.
“We have people living in aged care facilities who generally don’t want to be there… They’re not treated like it’s their home. They’re locked in. They can’t get out into the community,” she said.
“We’ve taken to thinking it’s okay to incarcerate people for getting old or for having dementia,” she said.
Senior counsel assisting the commission, Peter Gray QC, closed the hearing, saying the overriding theme of the Sydney hearings, which were based around dementia, were the need to respect the humanity of people living in residential aged care.
“The constant theme that emerged from the witnesses in this hearing was the need to respect the enduring humanity of the people in care, no matter how far their cognitive function might have declined and no matter how challenging it might seem to be to care for them.
“Older Australians who move into residential care do not leave their rights at the door of the facility and a resident living with dementia is entitled to respect and dignity and the freedom to live their life as they choose to the greatest practicable extent, as much as any other human being,” he said.
Friday was the last day of the royal commission’s Sydney hearings. The next hearings will take place on 17-19 June and 24-28 June in Broome, and will focus on aged care for indigenous Australians, person-centred care, and aged care in remote locations.
In relation to psychotropic drugs being administered with the authority of family/friends, it does not matter one way or another in nursing homes because they do what they want. I absolutely refused the administration of such drugs to my father and yet they went ahead and did it anyway. When I saw that my father was almost comatose I approached the Director of Nursing and she denied it. Because of his condition, I immediately took him away from the facility and straight into hospital where they confirmed he was overdosed with such drugs. He actually had DVT in his legs which had progressed to his lungs and that was the cause of his agitation. Had I not removed him from the facility he would have died.
The result of this was that the Director of Nursing telephoned the hospital and wanted to section him under the Mental Health Act so that I would have been removed from his care etc. and my rights as his enduring guardian would have been nullified. Fortunately, the hospital refused to do this but the Director of Nursing then urgently applied to place him under guardianship under false pretenses. I won the case and removed him that day from the institution.
I placed my father there for respite because I was totally sleep deprived as I cared for him on my own for over 3 years without a break. I did, however, visit him every single day for a minimum 5 hrs. per day whilst he was there so I saw everything that went on in that institution during those 5 months – it was a nightmare.
I cared for my father for another 5 years in my own home and I would NEVER EVER place someone in an aged care facility no matter how much it cost me physically or financially. They are nothing but warehouses for society’s most vulnerable, some worse than others. The Aged Care system is broken and should be completely reformed. There also needs to be legal punishments to protect the vulnerable and their families from the dictatorial behaviour and bullying by the service providers. For the most part aged care facilities are money spinners for providers and jail sentences for its inmates. God help the poor souls who do not have advocates on their side to protect them. I have seen enough of them to know that I will do what it takes to ensure that I will never end up in one.
I also feel great empathy for the few good nursing staff who really care and want to do the right thing but are prevented from doing so because of management demands. Eventually they leave because they can’t stand to see what is going on and they are powerless to stop it. And so we are left with ……….. I don’t need to spell it out.
Always an excuse, a nurse should be present with a doctor when he is visiting patients to contact family/POA if need be. Instead of doctors asking nurses to contact family to sign consent forms next time they come to visit the nurse should call family/POA and get consent over the phone or if uncontactable via phone how about email. At least if medicine is administered by nurses to patients they have proof that they tried to contact family or POA’s. Give the family/POA 48? hours to deny consent, if the family doesn’t respond then proceed with the doctors orders. Sadly I too know of patients being administered medications without family consent, but in these cases I know the family were never contacted. So sick of excuse after excuse, there is always a way to go about things and the new law reform should be making these situations easy and cut and dry. Figure it out your supposed to be professionals……