Sepsis is a life-threatening condition caused by the body’s immune response to a bacterial infection that has entered the blood stream. It leads to damage of the body’s tissues and organs. According to The George Institute for Global Health, “It kills more people than prostate and breast cancer, but six out of ten Australians have never heard of sepsis.” This deadly disease affects more than 30,000 Australians every year, and kills up to 5.3 million people annually around the globe. For every three people that come down with sepsis, one will die.
In a recently published quality standard, NICE declared that patients exhibiting signs of sepsis must be seen by a senior doctor and need to be treated within one hour with antibiotics and intravenous fluids. If at high risk, they should be seen immediately. The medical staff is also required to give patients that are assessed as low risk information regarding symptoms and when to receive medical care.
This declaration follows a report by the National Confidential Enquiry into Patient Outcome and Death that stated “40 per cent of people admitted to [the ER] with sepsis did not have a timely review by a senior clinician.”
Any infection—bacterial, viral, fungal or parasitic—can trigger sepsis. This infection can be caused by anything–from a bug bite to pneumonia. Those at higher risk include the very young and the very old, those with chronic illnesses such as diabetes, cancer, heart disease and COPD as well as people with impaired immune systems.
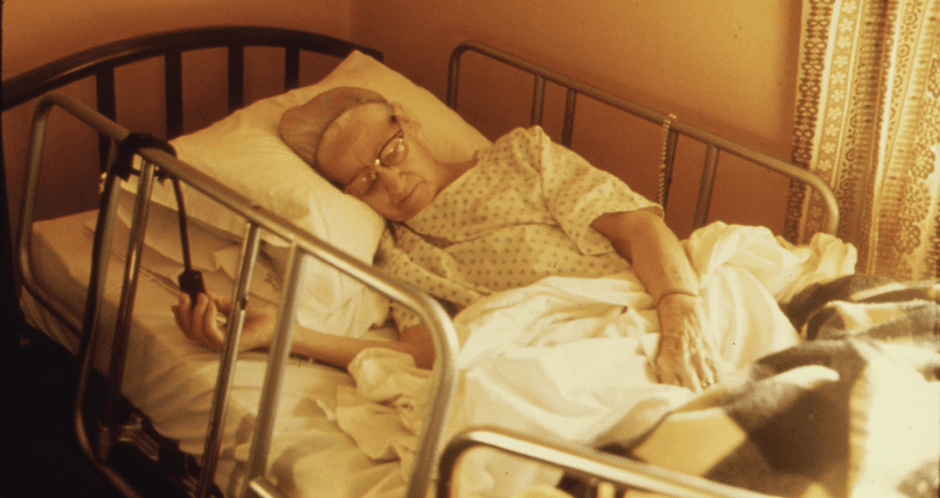
For the elderly, the most common infections that trigger sepsis are pneumonia, urinary tract infections, and pressure sores from sitting in a wheelchair or lying in a bed. What makes it even more difficult in this age group is that the infections themselves are often easily missed. While a younger person will show signs of a urinary tract infection that includes frequent urination and a sense of urgency, an elderly person’s first symptom may be confusion. The signs of pneumonia in the elderly can also be very subtle. Due to decreased lung function, their cough may be minimal and shortness of breath hard to detect.
Because early diagnosis and treatment is so critical, it’s important to know the signs and symptoms of someone who may be developing this disease. Sepsis can worsen quickly, leaving little room for a missed diagnosis. For family caregivers, it can make the difference between life and death for their ageing parent. Unfortunately, the signs are not always easy to detect and can be misinterpreted as symptoms associated with other diseases such as the flu. Early signs include the following:
Severe symptoms can develop quickly and include the following
Sepsis can leave those who have been affected with severe disabilities. A report in Emergency Live referred to Korina Valentine, a sepsis survivor who ended up as a quadruple amputee. In addition to missing limbs, long-lasting effects include kidney failure, memory loss, cognitive decline, chronic pain and fatigue.
For the elderly, a bout with sepsis can leave them unable to perform the daily activities of living. Primary family caregivers are often faced with these additional responsibilities.
If you believe that you or a loved one has developed an infection, treat it promptly. Even the smallest scrape warrants cleaning with soap and water and the application of an antibacterial ointment. Proper and frequent hand washing also decreases the risk of infections. It is always best to veer on the side of caution. If you believe your parent may be exhibiting any of the signs of sepsis, obtain emergency medical care immediately.
5
4
I’m a 75 year old and terrified of getting elder and nead care in latter years. I read all you column and than you. Regards Esterperegi