
Recognising when the health of an aged care resident is deteriorating is fundamental to ensuring the person receives the care and treatment they need.
It’s a sign that intervention is needed. When deterioration occurs it’s important it’s recognised promptly, and that appropriate action is taken.
But how can aged care workers observe the often subtle signs that a person is deteriorating, especially if they are agency staff and seeing different people every day, or if they are new to an aged care home?
A member of HelloCare’s Aged Care Worker Support Group recently asked if there is a structured way to identify if a resident is deteriorating. We reached out to an expert in the field to find out what tools they recommend, what to look out for, and what carers can do when they find that a person in their care has begun to decline.
Kate Reed is a palliative care nurse practitioner and works with Palliative Care Australia. She has worked in aged care homes for over a decade. When we spoke earlier this week, she began by telling HelloCare that the first thing you will notice when a person is deteriorating is a change in their habits.
“You might think, ‘Mum’s been in bed for two days. She might have a bad day every now and again, but two days is a bit strange, and she didn’t eat her dinner last night and she didn’t want her breakfast.’
“These sorts of changes can be really telling that something is going on,” Ms Reed explained.
Early signs of deterioration to look out for include a sudden lack of care about appearance, stopping attending group activities, and reminiscing about the past.
More than two trips to hospital within a six-month period can also be an early sign of deterioration, Ms Reed said.
In the later stages of deterioration, people might experience more fatigue than usual and they might begin to lose interest in food.
“It’s really important to keep their mouth clean and moist, but they’re unlikely to be wanting to have food” when their condition has progressed to this stage, Ms Reed said.
They might have nausea or a change in their bowel movements too.
People with a malignant disease may notice an increase in symptoms, for example, there might be an increase in pain or an increase in fluid in their bodies causing swollen feet because their heart isn’t working so effectively.
Some people go from being in “lots of pain to being in very little pain,” Ms Reed said.
It’s probably not surprising that distress can also be a common factor at this stage.
“The level of distress a person is having with their symptoms speaks to us about how fast you need to move,” Ms Reed said. “If they do have distress, it’s really important to involve specialist palliative care at that point.”
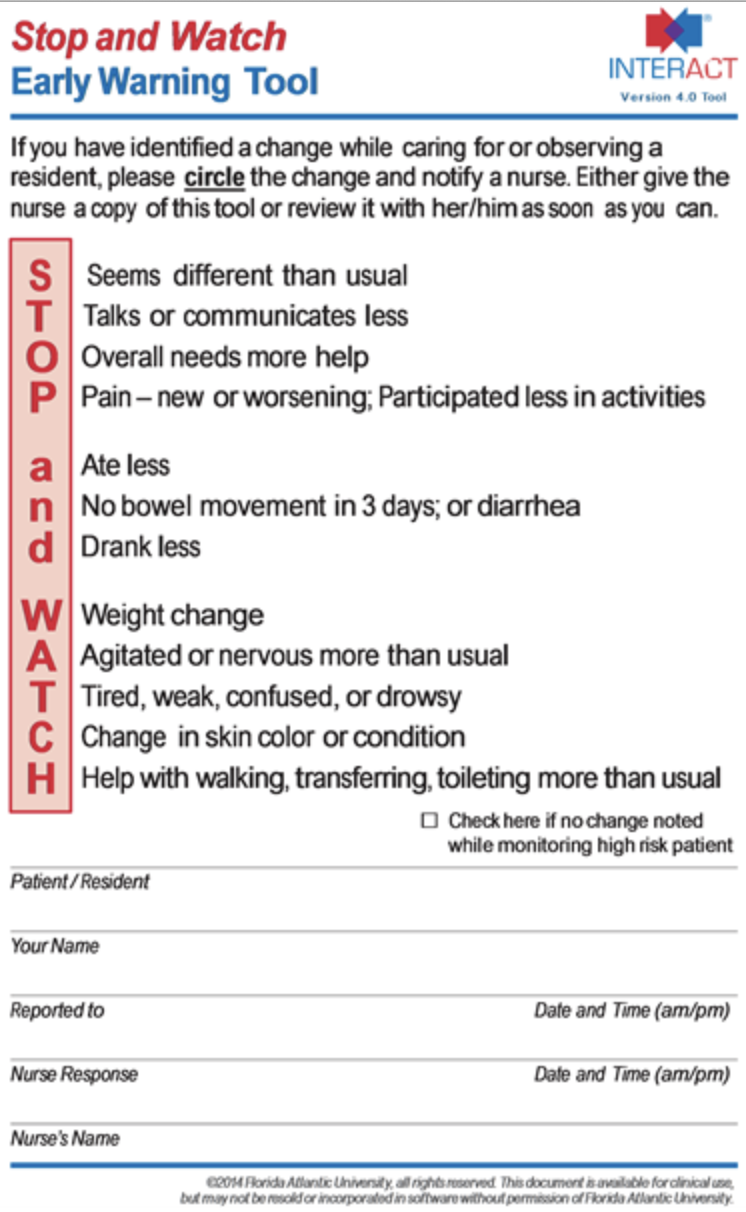
Members of the Support Group said the ‘Stop and watch early warning tool’ provides a framework for monitoring changes in a resident.
It prompts staff to be alert for potential changes in condition and provides a simple, clear way to communicate changes to nurses.
Ms Reed recommends the ‘Supportive and Palliative Care Indicators Tool’ – also known as SPICT – for regular assessments. These checks can be “repeatable and regular” so you can check a person over time and see how they have deteriorated.
Carers can use the tool to assess if the resident has unmet support and palliative care needs, and it can trigger important conversations and reviews to help plan future care.
Ms Reed also said asking the ‘surprise question’ – asking if you would be surprised if the person was to die in the next 12 months – can also be helpful.
If the answer is yes, then little needs to be done immediately other than some advance care planning.
But if the answer is no, Ms Reed recommends making sure the advance care plan is up to date. Begin having ‘goals of care’ conversations with the health team and loved ones about what the person wants, such as where they want to be to die and what interventions they would like.
In the sad situation where it appears the person is likely to die soon, Mr Reed says it’s important to contact their GP.
“The GP is the primary care provider and they will often have a really good idea of where the patient’s at,” she said.
A case conference with the GP and specialists can determine what the person’s prognosis is, what to expect in terms of symptoms, and what can be done to support the person. It’s about making sure the person is not going to suffer, so that everyone is informed, and so that loved ones all have the same picture and there is therefore consistency in the plan.
“You can have a really great plan, but if it’s not communicated to everyone then it can fall apart because there’s a lot of emotion and stress at that time,” Ms Reed said.
‘Terminal care planning’ is done in the last days to week, Ms Reed recommended, and involves talking to families about what to expect.
At this stage of life, the person’s consciousness will decline, and they’re unlikely to be able to swallow. They may experience confusion and disorientation. Alternative measures have to be taken, such as using injections and infusions, to make sure they receive the medication they need “so they’re not suffering”, Mr Reed said.
It’s important that family are informed about what dying will look like, and that the deterioration and changes they are seeing are a normal part of the dying process.
Many people die without palliative care, but at this stage of life people still need to be assessed regularly to identify what symptoms they are experiencing, and to make sure symptoms are being addressed properly.
Plans need to be in place by this stage. For example, it’s important to know what to do if the resident doesn’t want to go to hospital. Who’s the first person staff should call if something goes wrong? Who’s the enduring power of attorney?
“Those sorts of plans need to be in place way before they’re needed,” Ms Reed recommends.
Recognising the signs of deterioration as a person’s disease progresses does become easier and more acute with experience, Ms Reed said.
“I’ve looked after so many people who have been dying and have died, and also people who have been living with their disease for quite a long time. Treatments are better and people are living longer… but it still isn’t an exact science,” she said.