The federal government has launched an independent investigation and the state government has mandated staff ratios in the wake of the emergency evacuation of residents from Earle Haven Retirement Village last week.
Minister for Aged Care and Senior Australians, Richard Colbeck, announced an independent inquiry today into the forced evacuation last week of nearly 70 frail residents from the Earle Haven Retirement Village.
Minister Colbeck said he was “angered and appalled by the terrible and unprecedented events” that took place.
“Residents should not have been put in a situation where they were forced to be relocated because they were left without the care they so rightfully deserved,” he said.
The government has appointed Kate Carnell AO to lead the investigation. Ms Carnell co-conducted the Carnell Patterson review on aged care.
“I look forward to Ms Carnell’s report,” Mr Colbeck said.
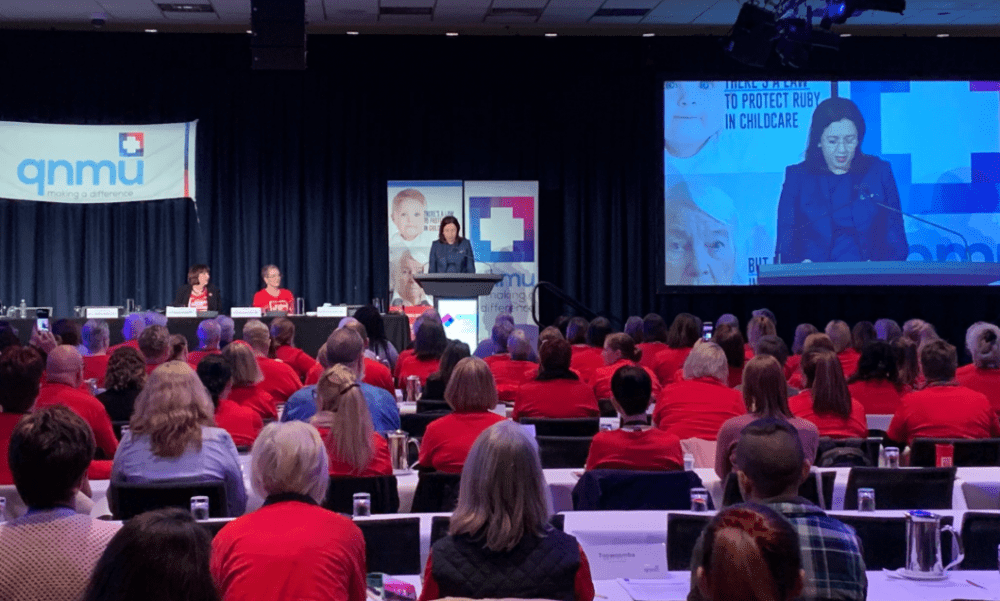
The announcement came only hours after Queensland premier Annastacia Palaszczuk revealed her government will make minimum nursing hours mandatory, and by the end of the year the figures will be published online and made available to the public.
The Queensland government has moved to mandate a minimum 3.65 nursing hours per resident, extending hospital nurse-to-patient ratios to the aged care sector.
The premier said mandating staff ratios in aged care is the first scheme of its kind in Australia.
Queensland Nurses and Midwives’ Union Secretary, Beth Mohle, told HelloCare the union was “thrilled” by the premier’s announcement.
She said the government has agreed to mandate that aged care facilities have 30 per cent RNs, 20 per cent, ENs, and 50 per cent AINs or PCAs.
Ms Palaszczuk said, “Revelations at the Royal Commission into Aged Care and recent events at the Earle Haven retirement village on the Gold Coast have demonstrated how important it is for residents and their families to have comfort and confidence in the care they receive.
“We brought in mandated nurse to patient ratios for Qld hospitals. Now our 16 state-owned aged care facilities will all publish their ratios of nurses to residents by the end of this year.
“It should bring confidence and comfort to aged care residents and their families,” she said.
The premier is asking private aged-care facilities to voluntarily report staff numbers and contact hours.
“I want to see a public register so families and friends can have a look at that, that dictates very clearly (which) facilities (are) offering minimum contact hours,” Ms Palaszczuk said.
Those who don’t provide the data, will “have to explain to the residents and to the residents’ families why they have chosen to hide that data.”
The premier is also calling on the federal government to mandate staff ratios for private aged care operators, of which there are around 400 in Queensland.
“We will be urging private aged care homes to do the same, but as they are the responsibility of the federal government, only it can introduce a mandate for the sector. I’m calling on them to act as we have,” Ms Palaszczuk told media.
“Let me make something clear. Our aged care sector is booming, and our elderly residents are not getting the full care they deserve,” the premier said.
“How do I know this? Because people have spoken to me directly about it. I had one woman who held my hand and said you have to help us. She said to me she could not breathe properly and it took over one hour for someone to come and see her.”
Ms Palaszczuk said people living with dementia often don’t “have a voice” and some elderly residents do not have family or friends to “check up” on them.
“I want to see a public register so family and friends can have a look at that facility, and there’ll be a transparency about it that shows clearly that the nursing home is offering minimum contact hours.”
According to the QNMU, one registered nurse was left to look after 68 residents on the day the Earle Haven Retirement Village aged care crisis unfolded.
Residents at Earle Haven received an estimated 2.73 hours of care a day – rather than the recommended 4.3 hours.
QNMU Secretary, Beth Mohle, said off-duty nurses and other staff rushed to the facility to help residents and provide support as the evacuation took place.
“This was a crisis not of their making, but once again vulnerable residents and hard-working staff bore the brunt of critical flaws in the regulation of aged care,” Ms Mohle said.
“Earle Haven nurses… should be commended for their efforts,” she said.
Ms Mohle said private aged care providers often “cried poor”, but Australia’s approximately 900 aged care providers receive around $18 billion from the government every year.
They also receive a deposit of up to $500,000 per resident, per bed, and up to 80 per cent of each resident’s pension, or up to $800 per resident, per fortnight.
“They do not have to publicly report how a single cent of taxpayer or resident funds are spent or ensure that funding is spent on direct care for residents,” Ms Mohle said.
Aged and Community Services Australia has asked the Queensland Government to consult with the industry about today’s staffing levels announcement, and has requested a meeting with the government.
ACSA Acting CEO, Mr Darren Mathewson said, “Previously, the Queensland Government acknowledged that staffing ratios needed to differ from centre to centre based on the individual and complex needs of residents.”
“ACSA is concerned about the nature and language of today’s announcement that seems to fail to acknowledge this.”
“ACSA acknowledges the call for transparency and more meaningful consumer information, so residents and their families have access to relevant information, however, the federal government is already active in this space. There is a risk of duplication and confusion.”
Leading Age Services Australia has called on the Queensland government to take a national approach to staffing levels in aged care, rather than going its own way. It also has called on great consultation with industry.
LASA said outcome based measures, such as that based on consumer feedback, are the most useful guide for consumers to identify which services will best meet their needs.
“More staff with high levels of qualifications (at Oakden) did not translate into high standards of care,” a statement from LASA said.
Image: Facebook.
If you mean registered nurses call them that, if you mean enrolled nurses call them that, otherwise you are talking about carers who have little training and no responsibility.
The Earle Haven disgrace is a real test for regulators.
Someone made decisions which totally ignored the safety and rights of residents.
If regulators do not declare those people to be “disqualified individuals” and apply the maximum sanctions against the Approved Providers, then the Minister will need to replace the senior managers within the regulator.
There can be no excuses, no special pleading by the lobbyists and lawyers.
The Earle Haven residents rights and expectations have been trashed.
……”The premier is also calling on the federal government to mandate staff ratios for private aged care operators, of which there are around 400 in Queensland”……
The Premier should also publish the cash flow and balance sheets of each of the State owned facilities and show how they run them without propping up the wages with Qld Health (Qld Taxpayers) money? Private operators do not have the luxury of a bottomless pit of money like state owned facilities.
Some time ago I wrote to Ken Wyatt outlining the reasons why staff ratios should be mandated in aged care, specifying registered nurses, assistants in nursing and nurses. His response to my letter was that he did not consider it a priority as it was not a main component in providing satisfactory care. That he no longer has the aged care portfolio is a blessing. Let’s hope he has a better grasp of indigenous matters and does not fail them like he failed the aged care sector. The Royal Commission’s transcripts of the Brisbane hearings address this issue of staff ratios and only confirm my view (and many of my colleagues) that Mr. Wyatt’s departure from his previously held portfolio was not only timely but also necessary.