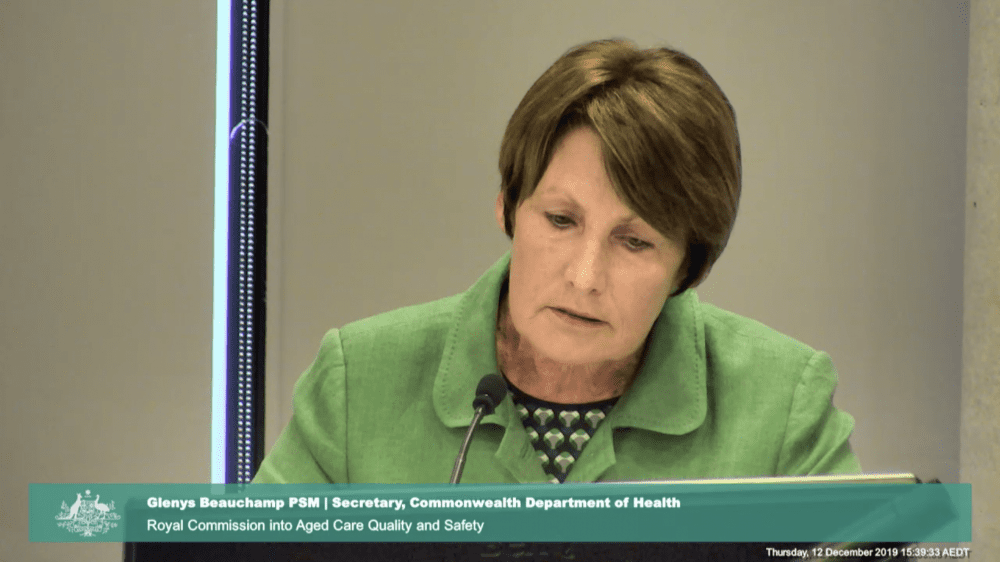
A senior official from the Department of Health has disagreed with the royal commission’s assessment that GP services in aged care are at times not meeting the demands of residents.
Counsel assisting the royal commission, Peter Gray QC, told federal secretary of the Department of Health, Glenys Beauchamp, about a survey of aged care facilities. The survey found 92 of 96 facilities had an ‘urgent’ or ‘immediate’ need for the services of a GP, in other words, a resident needed to see a GP either today or now.
Ms Beauchamp replied that she didn’t believe access to GPs was a problem.
“Access to GPs in a global sense doesn’t seem to be an issue. That doesn’t mean there aren’t urgent and hotspots that might emerge at particular points in time or… in particular areas,” she said.
“There’s certainly been not only an increase in the number of GP services going into residential aged care, but… we have about 50 per cent or 54 per cent of the 37,000 GPs that are providing services in residential aged care facilities,” she said.
Mr Gray said with only around 50 per cent of GPs providing services to residential aged care, “when you move from the community into residential aged care, you’re not going to have continuity of care from that same GP.”
Ms Beauchamp disagreed. “Well, no, you couldn’t draw that conclusion,” she said.
Mr Gray suggested there should be clearer delineations of responsibility between the health system and the aged care system.
“I suggest it can be difficult to know who bears the responsibility for making sure that that person obtains the health care that they need,” he said.
The evidence around the issue was “quite concerning” and “obviously a failure within the system”, Ms Beauchamp agreed.
Mr Gray said there is no obligation for aged care providers to arrange for remote consultations with healthcare practitioners and no obligation to provide transport, make appointments, “things of that kind”.
“I agree with you, I think this needs to be strengthened,” Ms Beauchamp said.
Mr Gray said the limitation eroded providers’ ability to deliver “safe and effective personal care”, as required by standard 3.
“I suggest there’s a tension between delivering safe clinical care tailored in a person-centred manner to the needs of the person… and what service actually has to be provided… The standard seems to be asking for something that reaches beyond the service that the facility or the provider is funded to provide,” he said.
Ms Beauchamp said providers needed guidance around what was “practical and realistic”.
Mr Gray asked, “Should it not also be an obligation on the facility… to, in fact, obtain that care in a practical way? Not simply to make a referral or pass information, but to actually have more of a responsibility to ensure that the care is provided?”
“I think there should be more proactive care coordination,” Ms Beauchamp said.
Mr Gray and Ms Beauchamp agreed that aged care staff should take on the role of care coordinator or care coordination team.
They also agreed that the digitisation of health records should be made mandatory.
“Absolutely,” said Ms Beauchamp. But she added that healthcare workers should also be encouraged and trained how to use the system. “I think probably what’s more important is clinician behaviour and people who are providing input into My Health Record. I think that’s where we need to focus a lot of effort in terms of getting clinicians to use it and make it easy to use,” she said.
My mother passed away last December. Her GP did not visit and she suffered. We were told that a relieving doctor could not come or be called until after 6pm. We were not offered palliative care leading up to her death. We had NO support. We are still coming to terms with and still very upset with the manner in which our mother passed away. NO support from a GP, she was allowed to suffer and in her final 48 hours there was NO GP guidance or support. So distressing to watch. We promised her we would look after her and not let her suffer. She was ket down badly. Dont GPs care!!!!