Families have had to struggle to find out about the health of their loved ones living at St Basil’s Fawkner. They are deeply frustrated by what they perceive as buck passing, overly complicated bureaucratic processes, and an alarming lack of preparedness that is putting their loved ones’ lives at risk.
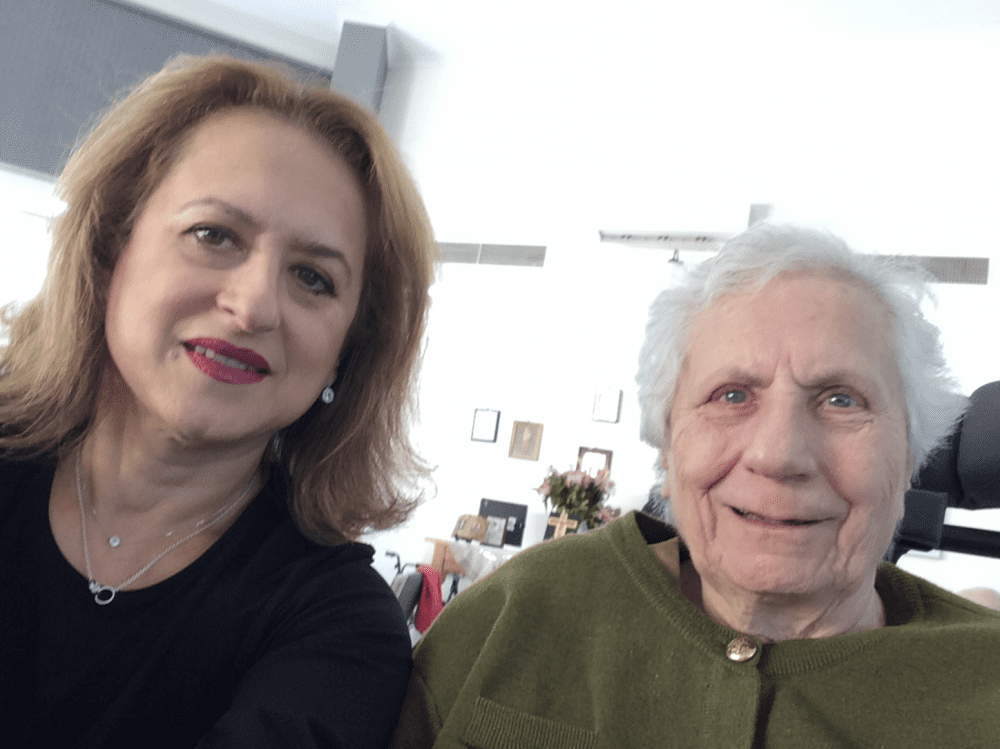
Christine Golding was denied communication or updates on her 84-year-old mother, Efraxia, for nearly a week. Being told she’d have to wait 24 hours for an update on her health, Ms Golding decided to go to the facility herself.
What she saw when she arrived at St Basil’s shocked her. Twelve ambulances were lined up on the grounds. Residents were being assessed to see who needed to go to hospital. There have now been 78 COVID-19 cases linked to St Basil’s Fawkner.
Ms Golding demanded to see her mother.
“We requested, demanded, persisted, and insisted that we go in, dressed in PPE. My mother has thus far tested negative and I’m terrified that that could change at any moment,” she told HelloCare.
But the staff said they could not let her in due to the “crisis” that was playing out inside.
Ms Golding decided to go around the back of the home and see her mother through the window. “I went to her window, took down the fly screen and banged on the window. The carer pulled the blinds open and then mum saw me,” she said.
Efraxia recognised her daughter, but was unable to speak. Her eyes seemed vacant and she appeared to have lost her ability to talk. Ms Golding dropped to her knees as the emotion of the situation overwhelmed her.
“There was no hope in her eyes,” Ms Golding said. “I thought to myself, what has this world come to. What has my mother ever done to deserve this?”
Up until that point, Ms Golding had been struggling to find out how her mother was. From the time the federal government stepped in to provide staff, and St Basil’s staff were sent home, it was often impossible to reach the home on the telephone, requests for information were ignored, and bureaucratic processes meant updates took hours or days to reach her.
Even though a social worker was allocated to Ms Golding to keep her informed of her mother’s condition, the social worker was based in Adelaide and only received an update on the residents each morning. Sometimes Ms Golding was told she’d have to wait 24 hours for a report on her mother, a period that seemed an eternity during the fast-moving COVID crisis.
For five days, Ms Golding had “no idea” how her mother was. Finally an update on her mother’s condition came through. “Oral fine. Comfortable. No pain.” No information was provided about a recent COVID test, leaving Ms Golding to assume she had tested negative.
“That’s unacceptable,” she said. The updates were merely “transactional”.
Last week Ms Golding said she wanted to talk to her mother on Facetime but was told she would have to wait until Monday. The delay prompted Ms Golding’s weekend visit to the home in person yesterday.
Ms Golding acknowledged that the staff were all trying their best, but her overriding impression was that they weren’t “skilled or trained” to handle such a complex situation.
The new carers that came into the home appeared to be inexperienced and they had not worked together as a team before, Ms Golding observed.
None of the staff could speak Greek, which was her mother’s first language, and to which she was increasingly reverting as her cognitive decline progressed.
The staff kept referring to ‘the patient’, which alarmed Ms Golding because people living in aged care facilities are generally referred to as ‘residents’.
Sometimes exchanges became heated. One nurse rudely asked Ms Golding, “What’s your issue,” after she enquired about her mother’s wellbeing. She replied, “I want to know who’s in charge. I want to know what the strategy is. And I want to know if my mother’s alive or dead.”
Ms Golding was concerned about St Basil’s handover to the new staff of information about medication, dietary requirements, and nurturing needs.
“You can’t hand that over in half an hour,” she said, noting that St Basil’s systems were still largely paper based.
Word spread of ‘horror stories’ within the home. One daughter went in to see her mother after she’d been told she was seriously unwell. When she arrived, she saw a pastie and a spring roll on her mother’s plate. Her mother, who needs her food pureed, was starving. “She wasn’t going downhill. She needed yoghurt, she needed water,” Ms Golding said.
“I’m also concerned they’ve got positive people with negative people next door. My mother’s door is open. There are people with dementia wandering around, going up to the COVID wing,” Ms Golding said.
“It’s chaos. I’m petrified for my mother. They are catching it because they don’t have proper controls in place.”
“I want to do everything I can to save my mother,” Ms Golding said. “My concern is that people will not get the right care… and that people will die from neglect and the shock of having strangers (the new carers) running in and out,” she said.
“This is human rights abuse. It’s a humanitarian crisis. This is clearly out of control,” she told HelloCare.
“Not only do we want to save our parents and give them the best chance of survival… we don’t want them to die from neglect or a broken heart. We also want to push for change. We should have been more prepared.”
Ms Golding now wants to get her mother out of St Basil’s and is hoping to get support from the government to do that.

John Atzarakis mother, Fotini Atzarakis, was eight days into two weeks’ respite at St Basil’s Fawkner when Melbourne went into lockdown.
When he rang the facility he was told he should have received an email about a staff member testing positive. But Mr Atzarakis said he never received an email, and nor did any other families.
Mr Atzarakis said he wasn’t surprised the virus spread within the home. “Behind the scenes it was like the staff were having a party. No gloves, no masks, they were just in groups together. No social distancing,” he said. However, since cases were identified, he said the situation has improved.
Initially, Mr Atzarakis was told only staff would be tested for the virus, and it was only after families protested that the residents were tested too. Last Tuesday residents were finally tested and two days later, Ms Atzarakis and his family were informed that his mother had tested positive.
Two days later she was transferred to Austin Hospital.
“Mum’s on oxygen now and she’s fighting for her life,” Mr Atzarakis told HelloCare. “She’s in her last days.” The family is not able to visit her.
Prime minister Scott Morrison in his press conference today said the government has been in touch daily with one family member of each resident. “That’s not happening. That’s lying,” Mr Atzarakis said.
In yesterday’s zoom meeting with the Minister for Aged Care, St Basil’s management and the Aged Care Quality and Safety Commissioner, Janet Anderson, Ms Anderson was asked who was responsible for the crisis at St Basil’s.
According to Mr Atzarakis, Ms Anderson said neither the federal nor the state government are responsible, the accountability lies with St Basil’s. “No one was was taking responsibility,” he said.
“My mother’s going to die. Passing the buck ridicules us,” he said.
Image: Christine Golding with her mother, Efraxia (supplied).