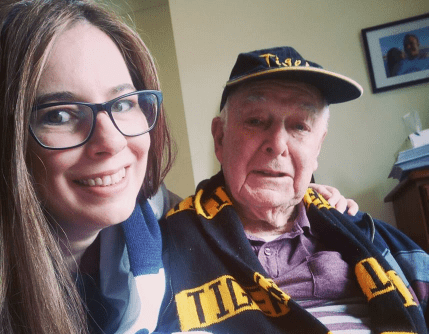
I’ve always had a close relationship with my Grandfather (Pop). When he was diagnosed with Vascular Dementia following a major stroke in 2016, there was no other choice but to place him in a high care dementia unit of a private aged care facility. Pop’s children live interstate now, so I thought it was important for me to visit him as often as possible. Even though he was different after the stroke, he was still the same kind and loving Pop I had always known. He still loved to joke around and he still enjoyed nothing more than to have a chat with me, listen to his favourite music from the 50s and 60s, or watch his beloved Tigers play footy over a nice coffee and cake. What started out as a decision to simply keep my Pop company during a difficult time has become a heartbreaking lesson on why we must introduce mandated staff ratios into all aged care facilities in Australia.
I was shocked and frightened for my Pop’s safety, and sometimes my own, by what I observed in his high care dementia ward in a private facility. When I went to visit I was regularly confronted by residents wandering around distressed, agitated and needing help. I often witnessed residents being verbally and physically violent to each other, staff members and visitors. I was particularly concerned that all this distress and agitation I was seeing in almost all of the residents there seemed to be going unchecked for dangerously long periods of time, because there was so often no nurses or carers in the main lounge of the dementia ward. When I checked to find out what the staffing ratios should be for a high care dementia ward I was shocked to discover that there are no mandated staff ratios in private aged care facilities. The Aged Care Act leaves it up to facilities to decide what appropriate staffing levels are.
The staffing ratios there were dangerously inadequate, dropping to two Personal Care Assistants (PCAs) on the floor and one Endorsed Enrolled Nurse (EEN) handling medications to care for 30-40 residents overnight, on weekends and on public holidays. Around 15 of these residents have dementia and require high care, and many of these residents do not walk and require two people to lift them. All it takes is one resident to require to be lifted by two people and you have zero carers on the floor. The RNs there barely even knew my Grandfather and I rarely saw them outside of their office.
Vascular Dementia is an incredibly cruel and unpredictable disease. Even though my Pop was usually the same sweet person that he’d always been when I was with him, he also had a lot of complex issues that required expert clinical care and behaviour management strategies from day one. That’s why he was placed in a high care dementia ward. His short term memory was dreadful and he would often forget what had happened just five minutes earlier. He was unable to walk, regularly experienced hallucinations and would frequently call out for help involuntarily, particularly overnight. He can only see out of one eye and hear out of one ear, so he has a lot of perception difficulties and can only really see people if they are standing directly in front of him.
Because the private facility he was at had nowhere near enough staff for somebody to comfort him, he was mostly ignored when he became distressed. There were quite a few times when I could hear him calling out for help from the carpark when I arrived and walked past several staff members to find him sitting in his wheelchair alone and still calling out for help. Any time I questioned staff about this situation, from PCAs right through to the facility manager, they told me “that’s just what he does” and considered my concerns to be dismissed. I always found that a particularly outrageous claim considering he very rarely called out for help when I went to visit him, unless he was also suffering from inadequately treated pain or an undiagnosed infection.
Pop certainly wasn’t the only resident in his nursing home who would get agitated and call out for help, but he certainly became the loudest and most persistent over the course of his two-year stint there as his dementia progressed and he often suffered from untreated pain and infections. It breaks my heart to think that almost every single person who knew him at that nursing home hated him. They didn’t see my kind, generous and funny Pop. All they ever saw him as for two years was “the man who always calls out for help”. Some of the residents would get so upset with how long he was left in distress that they would verbally and physically attack him, and of course he would respond in kind. I found it particularly distressing that the staff were so open in communicating that they found his distress and the subsequent bullying he experienced from other residents to be “so funny”.
He is now residing in a government run dementia specialised nursing home after a chest infection was ignored for three months by the staff at his private nursing home, despite the fact that my family did raise our concerns that he was suffering from a cold and seemed more unsettled than usual from January to March. His “problem” behaviours and agitation grew increasingly worse until he was hospitalised three times in March due to the same chest infection I suspect he’d been suffering from since January. Two of these hospital stays coincided with public holidays and I suspect these occurred so that the nursing home didn’t need to hire extra staff to care for him while he was so unwell. The manager of his “home” of two years refused to accept him back after his third trip to hospital, which is actually the most helpful thing they have ever done for him, as he is much more comfortable, clean and safe where he is now than he ever was there.
There are a total of eight residents in his new public nursing home and the staff ratios follow the Safe Patient Care Act. Despite the fact that my Pop’s health has deteriorated dramatically since the beginning of this year, he is so much calmer and settled with the extra attention his new nurses and carers are able to provide him with. They have been able to identify that he often just needs somebody to chat to him when he first becomes distressed, and they actually have the time to do that. And because he isn’t left alone in distress for such extended periods anymore, he has actually made some friends there. Every time I go to visit, the nurses and carers always have time to have a short chat with me and the residents are friendly, comfortable and participating in appropriate activities. I thought being sent to a nursing home for residents that private nursing homes can’t cope with was the worst thing that could happen, but it actually turned out to be the best environment for my Pop. I wish he’d been there from the beginning.
Mine and my Pop’s experiences in the private and public sectors of the aged care industry demonstrate that we must mandate staff ratios in private aged care facilities. Sarah Russell demonstrated that “If we want to improve the situation for residents, we need more registered nurses in aged care homes. When registered nurses are on duty, residents have better health outcomes, a higher quality of life and fewer hospital admissions.” Mandating staff ratios won’t wipe out all cases of abuse and neglect in aged care, but it’s the only way to move forward from the current broken system where profit comes before care and our elderly loved ones have to suffer for it.
Jade, Wow you covered all of my complaints/queries and some. I have had my wife in 3 nursing homes in 4 years and she is happy now in her last move (2 years) I support her 7 hours every day, she has alzheimers with Lewy bodies so doesn’t make a lot of sense but still recognises me.
I get into a lot of trouble at the nursing home because I constantly talk about the treatment methods you mention in your story, however this doesn’t stop me because I am the defence system she has, Many of the other residents families have reported the same problems at our monthly meetings but generally we are either considered “wingers” or radicals so in most case only small things are rectified.
Hi Bruce,
It can feel frustrating when your complaints don’t seem to be listened to, but you are definitely not a whinger for advocating for your wife. I have found that written complaints often gained a somewhat more satisfactory response.
All the best to you and your wife,
Jade
I agree with wha you say except it is not the need of more RNs but for carers who attend the everyday needs of the resident. RNs in my 15yrs experience are responsible for medications and often overlook what is reported to them by carers. It is the carerwho knows the needs of the resident not the person who administers medication.
You’re correct, John. RNs rarely spend time with the residents outside of clinical needs. I’d love to see a greater mix of both RNs and Carers in aged care so that carer’s could benefit from the experience of RNs and RNs could spend more time with the residents in there care.
Kind regards,
Jade
Well said Jade, what a shame Victoria is the only state with a Safe Patient Care Act and even there it only applies to hospitals or 4 named nursing homes (Govt run). https://www2.health.vic.gov.au/health-workforce/nursing-and-midwifery/safe-patient-care-act
Your wife is lucky to have you Bruce and the nursing home should be so grateful for your faithful support but I can understand how threatened they would feel having their shortcomings noticed. I agree with John too that the carers are the frontline and need more support, training in dementia care (statistically over 50% of residents are affected) and ideally a registration system like nurses so the few bad apples are weeded out and people are not forced into jobs they hate to get them off Centrelink payments. Together we can speak up enough until a critical mass is reached or Ken Wyatt is forced into residential care to really see how it is.
Thank you Jade for speaking up, and even after your lovely Pop’s passing you continue to advocate for the elderly. He was very blessed to have you there.
A good read, I left aged care last year after 17yrs. Yes I’m a Registered nurse. Not enough staff and I’m talking about trained staff who know how to care for our aged population, people with compassion, empathy and respect. A lot comes down to the people who run these facilities, they don’t listen, only think about the dollar signs. Can’t see things changing, which is very sad because our elderly deserve better.
I can relate to the above. My mother was
In a private age care home for 4 yrs,
Same treatment as mentioned above
Also staff not had enough training
Not enough Nurses it’s not there fault,
Its the providers of the age care home,
Lining there own pockets, before giving
Proper care to these beautiful human individuals in there last years .
Our Government needs to do more
To keep providers honest and show
Respect and proper care to our elderly.