
At Charlie’s Village, dementia patients of The Prince Charles Hospital in Queensland can visit the hairdresser, grab a coffee and escape the standard clinical setting right in the middle of their care unit.
A village-like community area was created within the hospital’s specialist dementia care unit outdoor space amongst nature fit with custom-built familiar facades such as a hair salon, bakery, café, general store, hotel, and post office.
Charlie’s Village was designed in collaboration with frontline clinicians and geriatricians with the support of The Prince Charles Hospital Foundation to create environments for patients to visit and feel confident and connected, allowing them to maintain some independence and mobility.
Since its opening in October, patients often have tea and coffee and spend quality time with their friends and family within this inviting outdoor space.
Research shows that environment can trigger behavioural changes in patients with dementia, so this addition will also assist staff in managing those behaviours as it allows for positive diversion.
Khera Kim, a Delirium and Dementia Service Nurse Practitioner at The Prince Charles Hospital said the village will help people feel more settled because they’ll feel like they’re at the shops or at a café rather than in an acute hospital setting.
“Bringing patients into an environment that’s more homely or looks like a normal community can help people feel better about themselves, and their quality of life can improve.”
Michelle’s 80-year-old father Neville, who has Alzheimer’s disease, had a stay in the dementia care unit in late 2023. She said this unique model of care provided a healthy distraction for her Dad who was often unsettled and prone to wandering.
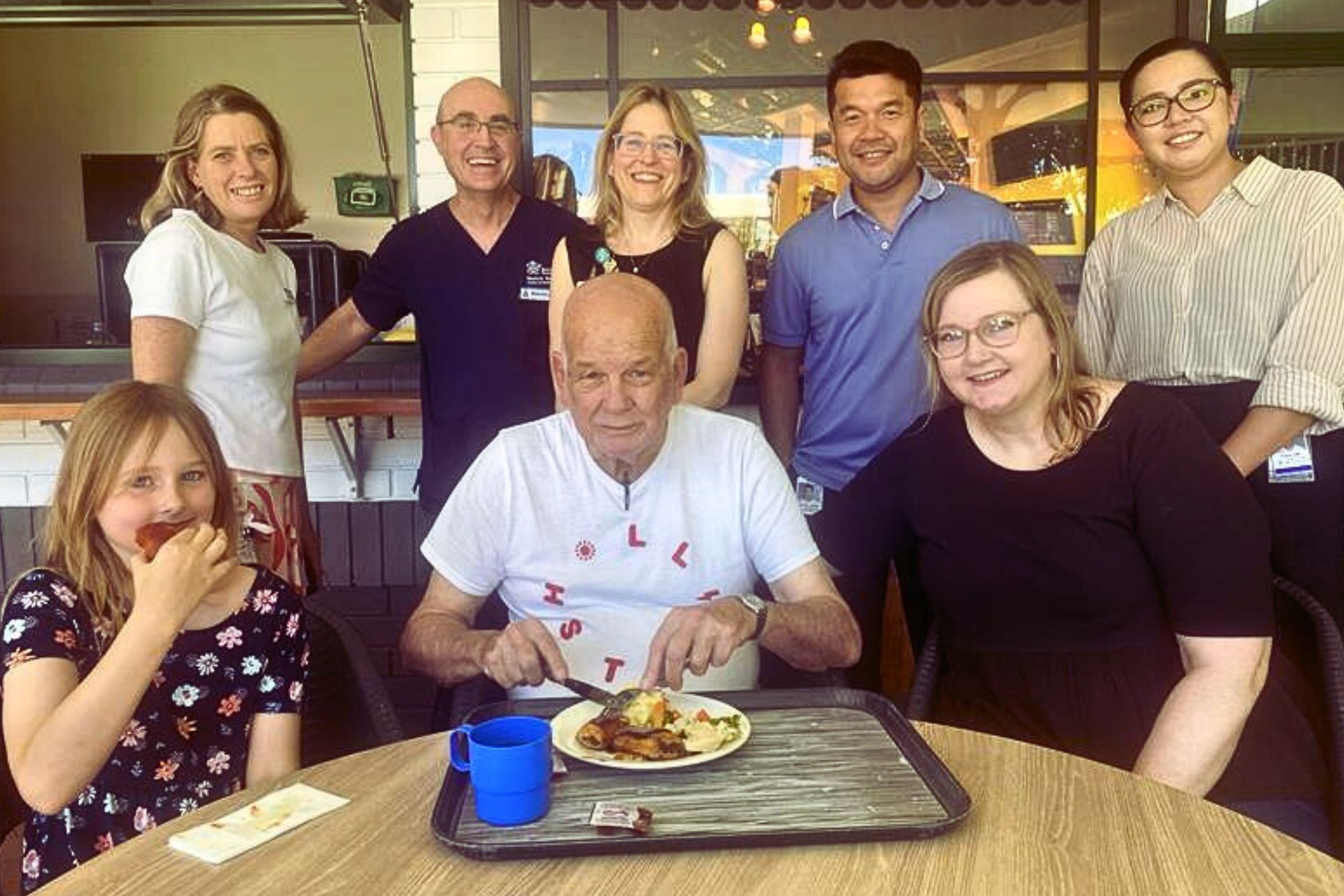
“Having the village there gave him something to focus on that felt like he was just up at the local shops. Here, he felt like he was where he needed to be as the space felt like a bustling community with other people and the amenities that kept his interest,” said Michelle.
“He also likes nature so he would comment on the plants or the visiting birds in the garden.
“The nurses there understood his desire to leave at certain times of the day, so they were able to redirect his focus (at times thanks to the village) and try to modify this wandering behaviour. This would reduce any anxiety and frustration Dad had from not being able to leave.”
Two years ago, Russ, 71, used to visit the unit to see his wife Noeline who lived with dementia. He has been volunteering at the unit ever since.

Inspired to carry on Noeline’s legacy in healthcare – who was a Senior Clinical Nurse Consultant during her working life – Russ also noticed on his visits that many patients didn’t receive visitors and decided he wanted to make a difference just like his wife.
To learn more about the initiative and The Prince Charles Hospital Foundation, visit www.thecommongood.org.au
Oh why is it called “Wandering Behaviour”. Neville is walking around, trying to understand his environment. Neville is going for a walk, plain and simple. The minute you have dementia and you walk around freely it’s labelled as problem behaviour and wandering, no, this is such an archaic attitude. It is nice to see that environmental gerontology has been considered at this acute setting, now match it with culture and language.