Two childhood friends from Myanmar, now husband and wife in Melbourne, are working together to create a better solution for palliative care in Australian hospitals.
In a system under strain and often unable to accommodate the personal needs of patients, industrial designer and inventor Dr Nyein Aung has teamed up with his wife, geriatrician and endocrinologist Dr Thinn Thinn Khine, to design a simple and cost-effective way to deliver a more patient-centred end-of-life experience.
Five nights on the floor
Growing up in Yangon, Myanmar, Nyein Aung was viewed as a trouble-maker.
One of the only people to recognise his potential was his English teacher, Julia Khine. ‘She was one of the only teachers who thought I was worth something,’ he says. ‘I didn’t know that I would marry her daughter one day, or cook her last meal, or be there as she was dying.’
Thirty years later in Melbourne, Dr Aung spent the last days of Mrs Khine’s life with her in a palliative care unit. Mrs Khine was visiting her daughter and son-in-law in Australia when she suffered a stroke.
In Burmese culture, people who are dying are never left alone overnight. In the standard palliative care room where Mrs Khine spent her last days, Dr Khine slept on the couch, while Dr Aung stayed on the floor.
It was during this experience that he thought ‘I could use design to help create better end-of-life care.’
A better concept for end-of-life
In Australia, the demand for dedicated palliative care spaces far exceeds the supply.
‘We know from the data that the majority of the population want to die at home or close to home, but people are dying in hospital because dying at home is still a huge task,’ Dr Khine says.
Because palliative care services are limited, end-of-life patients are frequently placed in acute or sub-acute hospital rooms instead.
These rooms are not designed to support a sense of togetherness, support, or communal grieving, and can be very isolating for patients.
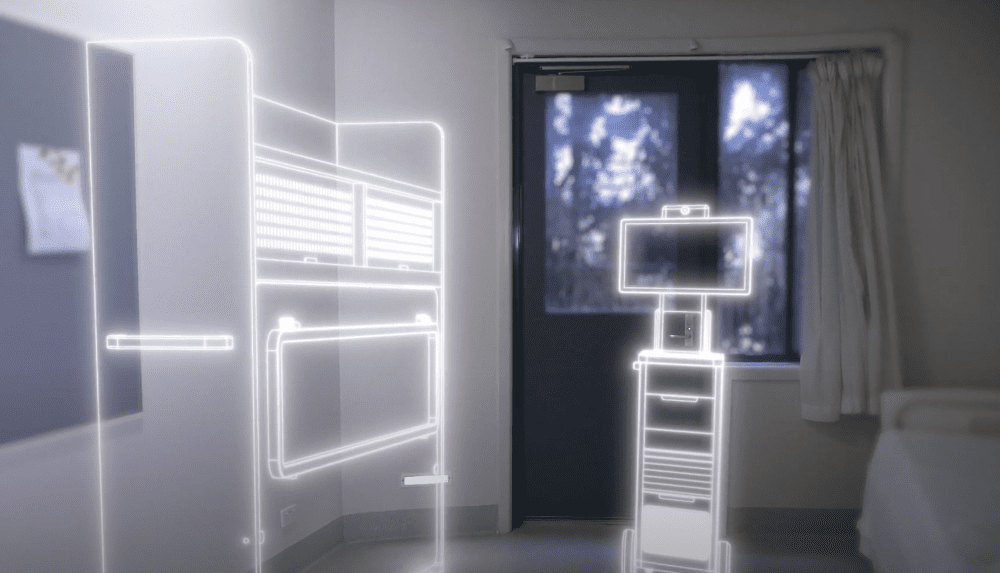
Dr Aung has created a simple, cost-effective concept to easily convert a standard sub-acute hospital room into a palliative unit that enables guests to sleep in the same room as their loved one.
The design includes a shelving unit that folds out into a bed, comfortably accommodating an overnight guest. The shelf space allows family and friends to bring in personal items.
Studies have shown that palliative patients want an average of five items with them as they die – normally sentimental and emotional objects such as photographs and heirlooms.
A ‘home-like space’ is a priority for patients, says Dr Khine.
‘A lot of people say, “Even if I couldn’t die at home, I would at least like to be in an environment that is familiar to me and be surrounded by people I love”, and things that remind them of themselves.’
The concept also includes a communication module, offering the opportunity for what Dr Aung calls ‘virtual togetherness’.
The module is a free-standing, sophisticated computer tray that can be used with personal devices and allows patients to connect with other family and friends who may not be able to physically visit.
The future of more personalised care
Even before her personal experience with her mother, Dr Khine was concerned about the largely institutionalised model of palliative care commonly seen in Australia.
She saw how isolating and impersonal the experience was for many patients. ‘As clinicians, we have these thoughts in our mind when we are interacting with patients,’ she says.
‘How can we connect design and medicine together to make this experience so much better? But we have no idea how to turn this into an actual product or design.’
Dr Aung has won awards for his designs that prioritise user comfort and he brought this philosophy into the palliative care project.
‘The current mode is, “Here’s the hospital, here’s the room, it is all set up”,’ Dr Aung says.
‘We want to challenge this idea.’
The combination of the space for loved ones to stay, the shelving for personal items, and the module for digital communication, is central to the project’s aims of allowing for personal connection, to matter how a patient prefers to receive it.
The project is receiving funding from Monash University and Creative Victoria.
Dr Hanmei Pan, Clinical Researcher and Consultant Geriatrician, is one of the doctors championing the project. ‘What we need is a design that reflects patient-centred care.
We, like many, operate on limited resources. This is something that turns a sub-optimal environment into an ideal environment to facilitate affordable end-of-life care,’ Dr Pan says.
Professor Barbara Workman, Clinical Researcher and Medical Director of Rehabilitation and Aged Care Services at Monash, is also working with Dr Khine and Dr Aung on the concept.
‘Being able to flexibly convert a sub-acute space to make it suitable for palliative care is a wonderful, cost-effective way for us to be able to meet our patients’ needs,’ she says.
By the end of this year, Dr Aung and Dr Khine hope to have built a functioning prototype.
‘The work is still in its early stages,’ Dr Aung says. ‘But we’re convinced that one day, the things we’re working on will make a big difference in palliative care.’
‘Losing a loved one will always hurt. I don’t think we can design or invent our way around that. But that pain doesn’t have to become trauma. That’s when design can be useful.’
See more here:
Image: KatarzynaBialasiewicz via iStock
I work in residential aged care, so the situation here is quite different when a resident becomes palliative, however when my own grandfather was dying in hospital it was a very lonely experience for him. He was in a shared room so we were not permitted to stay overnight & the other man in the room would complain if more than two people came to visit Pop at any one time so staff would limit our visits to two people & chase us out after only an hour. Complaints were made by the other occupant because my grandmother was crying so she was asked by staff to step outside the room if she needed a cry. All in all it was a terrible experience for everyone & sadly this was only 10 years ago, so we should have been able to expect a much more compassionate experience.
This is a most important contribution to palliative care, with worldwide value during this era of COVID-19.