
The standards of nursing homes in Australia have been in the public eye since the Oakden Aged Mental Health Care Service in Adelaide became embroiled in an elder abuse and neglect scandal, sparking reviews, inquiries and investigations across the sector. This was the most prominent of a series of incidents of abuse and negligence that eventually led to the establishment of a royal commission.
So what are the challenges facing nursing homes and why are they under so much strain?
In the 2017-18 financial year, more than 1.2 million Australians accessed some form of aged care service:
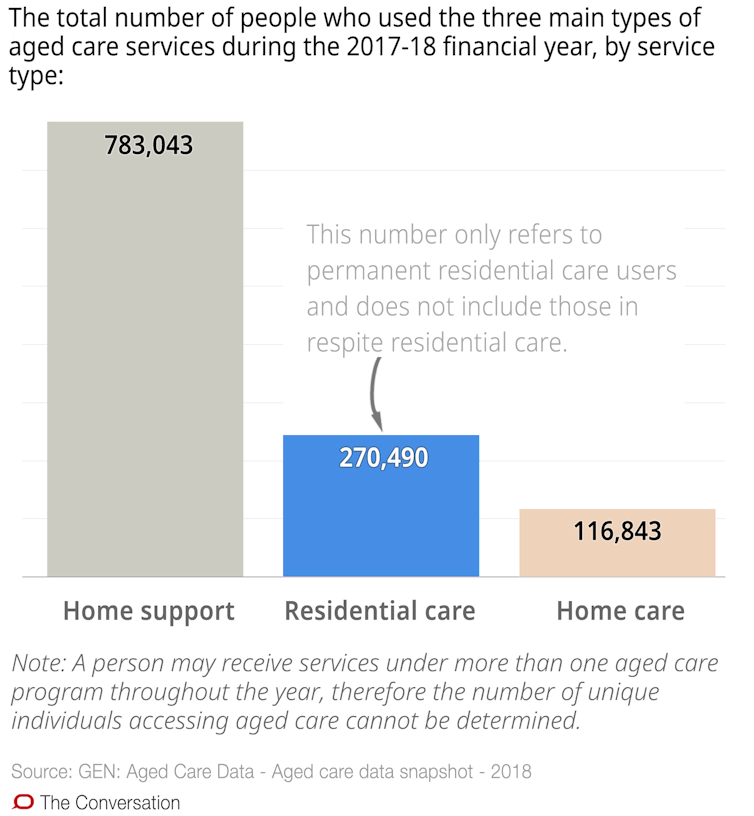
Residential care is the most resource-intensive category of aged care, providing higher level care to older Australians with complicated medical needs, those in the last years of life, and people who can no longer live independently in their own homes.
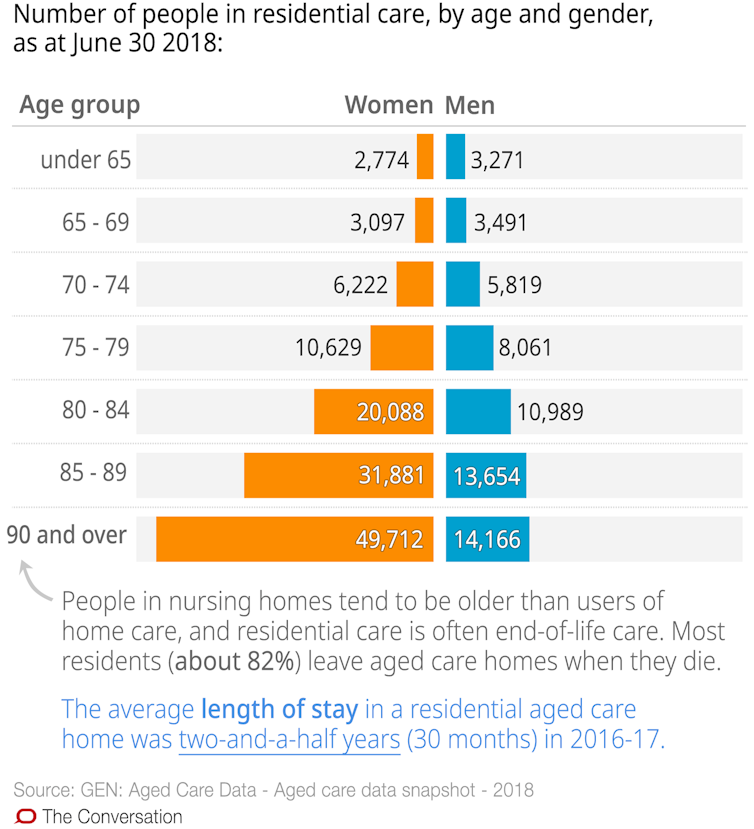
A large proportion of aged care residents are 90 and over. This reflects the increasing preference of older Australians to remain in their own homes longer, and only moving into residential care when home care is no longer adequate.
Australia has a relatively large proportion of older people, with more than 15% of the population aged 65 years or over, which has resulted in strong demand for aged care places.
In 2017-18, almost a quarter of a million Australians (241,723) were approved for residential aged care, but just over 207,000 places were available. This left a shortfall of 34,581 places.
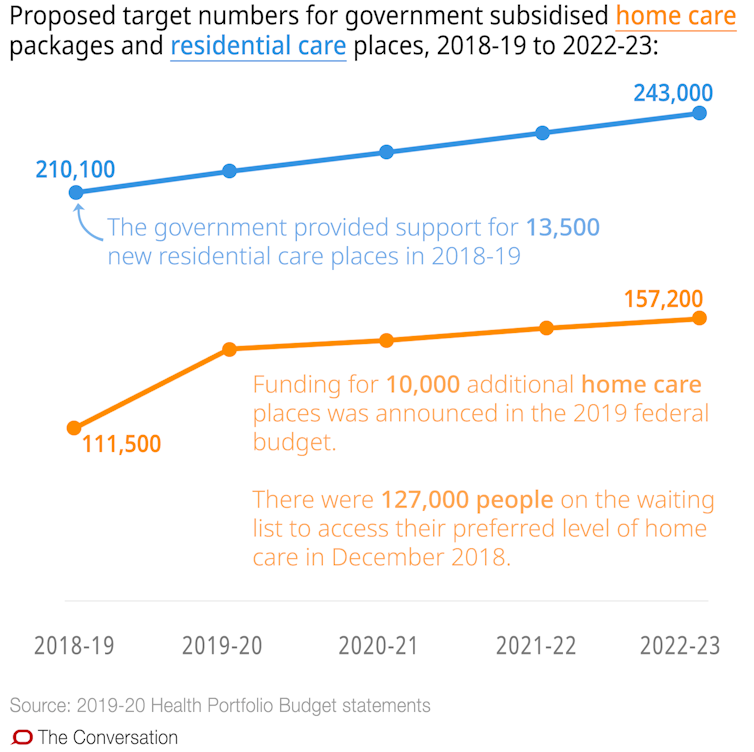
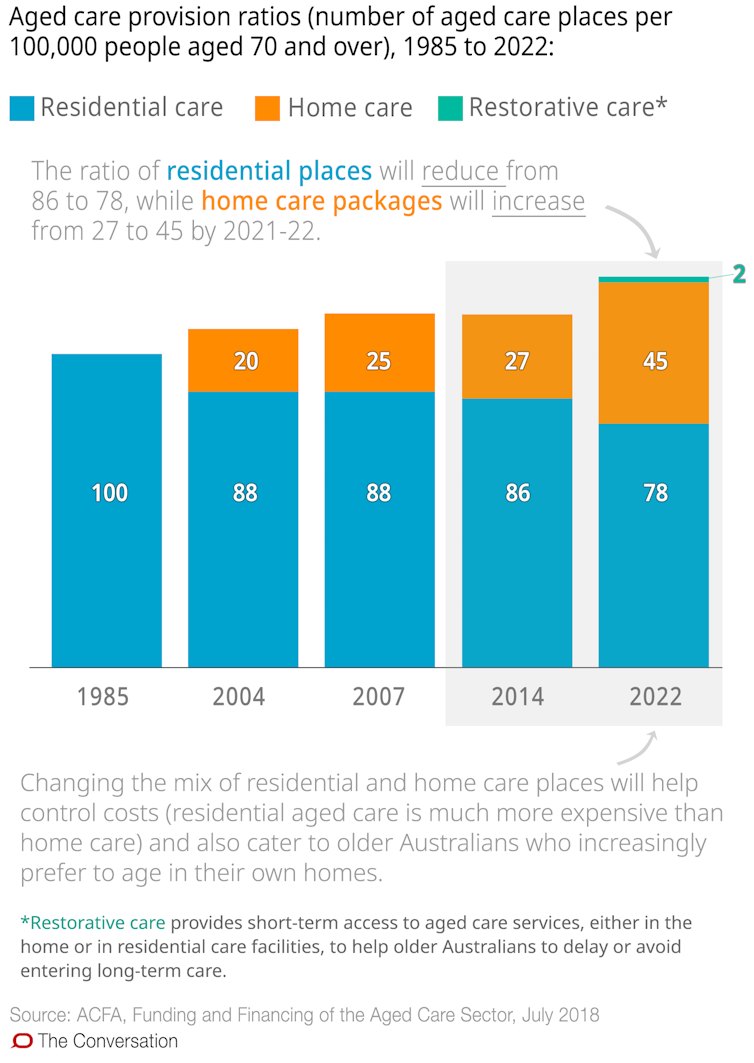
The supply of home care packages and residential care places is determined using the aged care provision ratio. The ratio will increase from its current target of 113 subsidised care places for every 1,000 people aged 70 and over to 125 places by 2021-22.
A 2015 survey by Bentley’s Chartered Accountants estimated that residents received an average of 2 hours and 48 minutes of care per day. The Australian Nursing and Midwifery Federation recommendsresidents receive 4 hours and 18 minutes of care per day.
The aged care industry does not currently have regulation related to minimum staffing levels, with the exception of a small number of publicly owned aged care homes Victoria.
The Productivity Commission estimated in 2011 the workforce will need to grow to about 980,000 by 2050 to meet the demand of aged care consumers. (And the population projections this estimate is based on have increased substantially since then, so this number may end up being significantly higher).
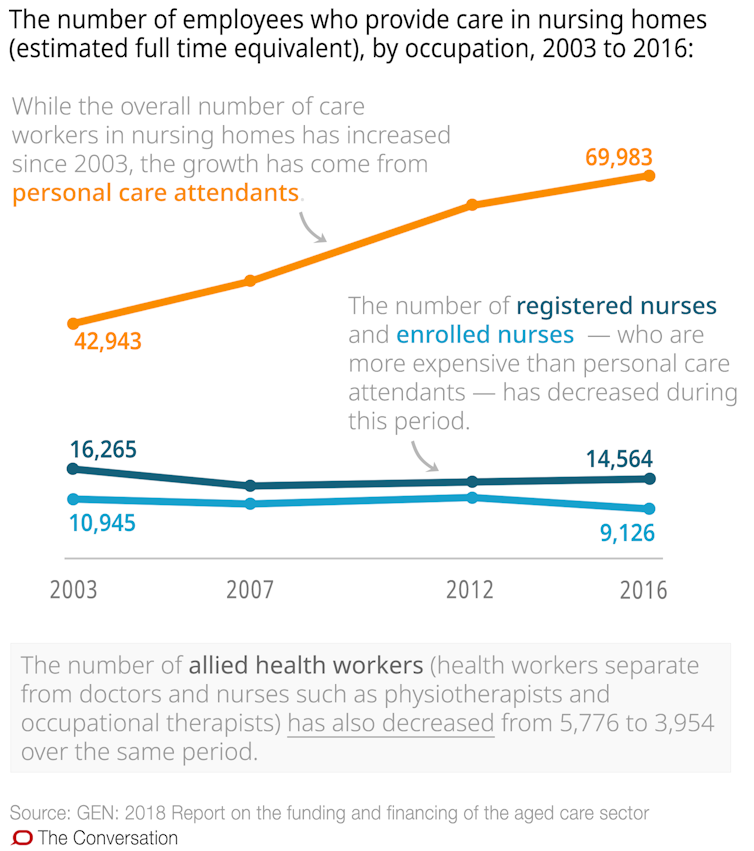
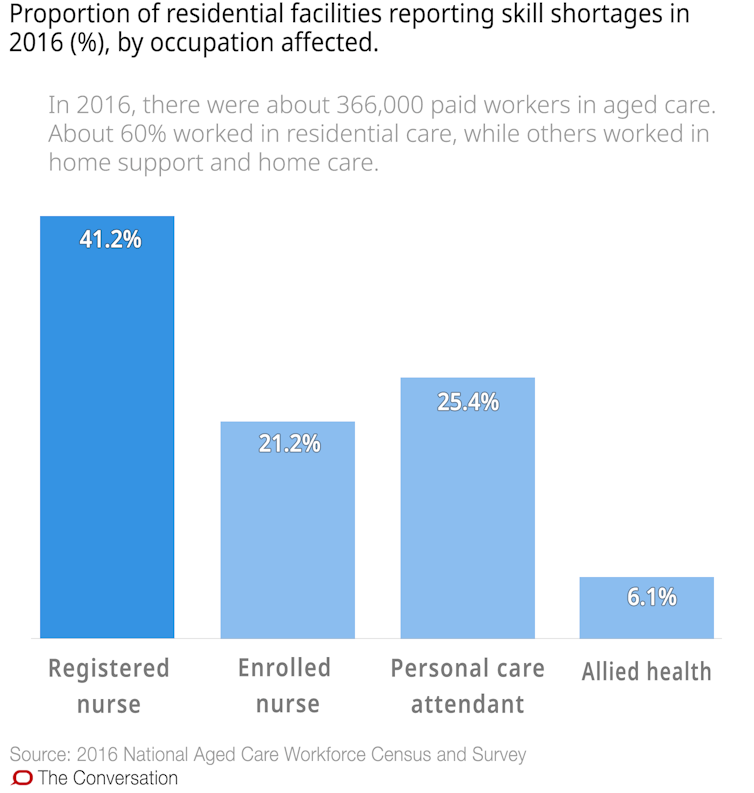
But providers are already finding it difficult to adequately staff nursing homes, with 64% of residential care facilities reporting shortages in 2016. And with employee costs representing 70% of the total expenses for residential care providers (an increase from 67% of total expenses in 2015-16), there is concern that residents will not be given proper care.
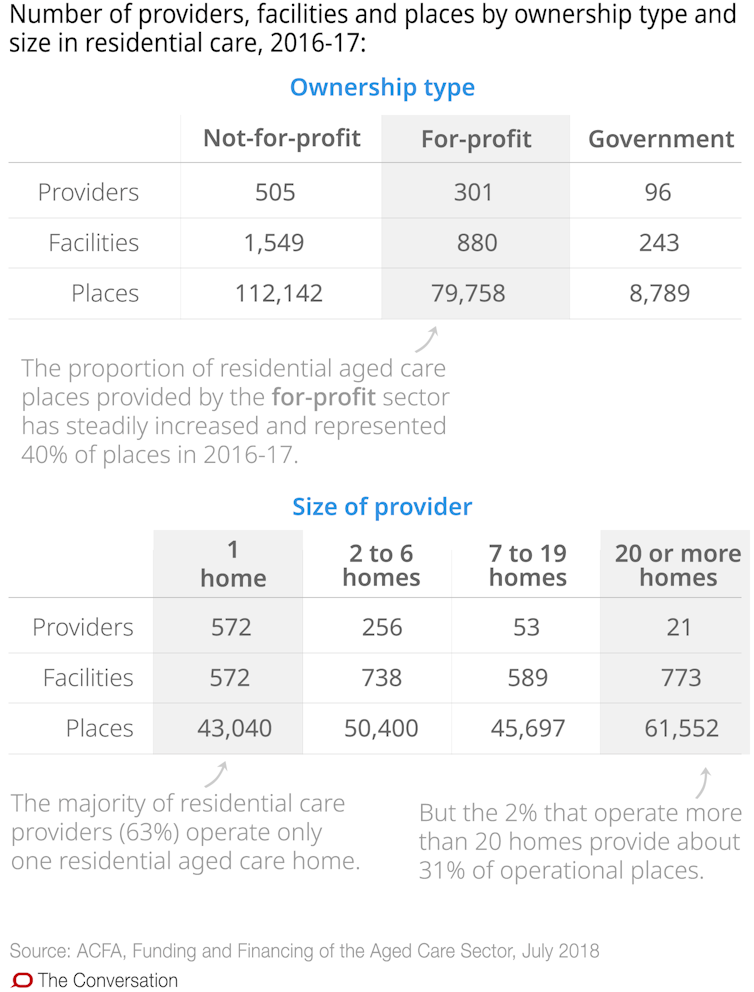
There were 210,815 operational residential care places as at June 30 2018, an increase of about 24,500 places in the last five years. Over that time, the number of providers has decreased from 1,034 to 886, mainly due to consolidation.
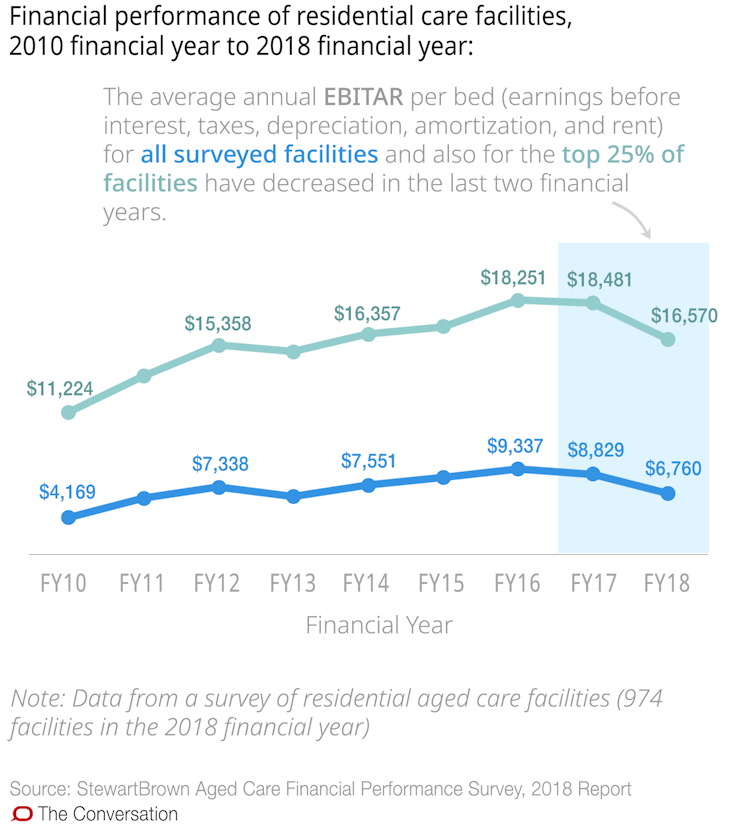
While profits (before tax) have almost doubled since 2012-13, only 68% of providers reported a net profit in 2016-17 (compared to 69% in 2015-16). A survey of more than 970 residential care facilities found 45% of facilities had negative earnings (before tax) in 2018, an increase from 33% in 2017.
Residential aged care facilities require government funding as well as resident contributions to operate.
Government contributions accounted for 67.3% (A$12.4 billion) of total provider funding in 2017-18, the majority (89%) of which is made up of the basic care subsidy.
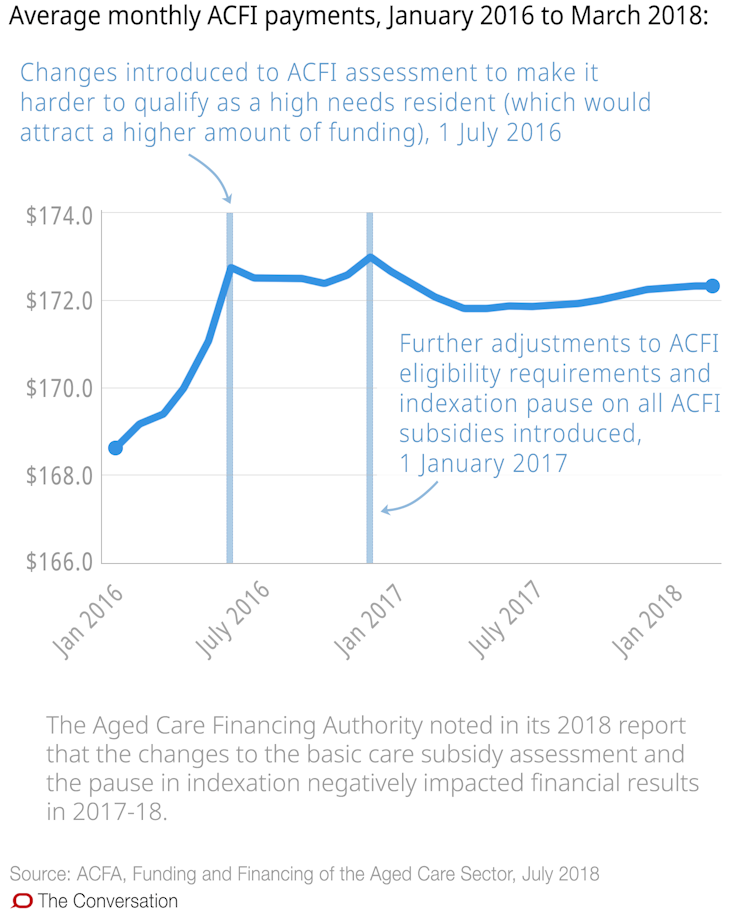
The subsidy is calculated for each resident based on their needs using the aged care funding instrument (ACFI). To care for a resident with high needs the provider will receive a larger subsidy.
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Hysterical headlines like this are deliberately misleading. You know well that there are no staffing ratios in aged care so to say that 2 out of 3 facilities are understaffed is simply scare tactics and you should lift your game.
When funding of Residential Care Facilities has been slashed to a point where half are running at a loss and the few making a profit have ROI of half a percent how does anyone expect growth, wage rises or confidence returning to the industry.
Where is the Government or opposition policy to correct the funding crisis? Only days until the election and shouldn’t the population of ageing know what their future holds?
On May 14 there is a National Action Day to highlight the abysmal financial future of residential aged care businesses.. The vast majority of facilities are delivering continuous excellent care but how long can they continue is anyone’s guess.
Let’s ask our pollies what they plan to do today, don’t let them tell you that the Royal Commission is working on it but that’s not true. They are not looking at funding but rather quality and safety. Plenty of reports already in place so liberals, fix what you have broken.
Do you have any data that proves half of the residential aged care facilities are running at a loss? I am aware the StewartBrown figures are selective but if the the top 25% can get an average of $16,570 per bed and 974 surveyed are still making $6,760 I call BS on rubbery accounting methods that are not transparent and often combined with other programs run by a provider. Especially not including interest on massive Refundable Accommodation Deposits paid by many, often more than their home was sold for.
I would like to see the data on that one too. I don’t believe some of these places are running at a loss. The company I work for are one of the biggest companies in the country. Always building new Aged Care facilities and incredibly flash if I may say so. They have recently revamped my facility at a huge cost. But no more staff! Let’s face it no Government is going to take it too far with the Royal Commission, that is why they washed their hands of the elderly in the first place because of the cost. yep they go on and on about training the staff. So that’s the problem? Pay the staff a fair wage and add a few more qualified RNs that can work on the floor like they do in hospitals and you may get a better quality of care and carers! the cleaners have now been hired to work for our place but only for 4 hrs a day. The AINs get their hands dirtier than the cleaners. We do everything. They don’t even have to clean around toilet bowls! Ains are expected to all the hygiene cleaning which is not as effective as you have in major hospitals. Disgusting when there are just as many bugs and hygiene issues as in any major hospitals. Shame Shame Shame on Aged Care and all Governments.
I am at a loss as to why Ken Wyatt has a position with the Liberal national party. He has done nothing for Aged Care. With all the information on staff shortages and neglect and abuse of both the aged and the staff he has not been in the public eye making a stand when it has been known in so many articles and media for years! You should have done your homework on that one Scott!