The National Disability Insurance Scheme (NDIS) is transforming the lives of hundreds of thousands of Australians with disability. For the first time, many can get the help they need to live more independently and be part of society.
And yet, the NDIS is failing people with the most severe disability: people who need housing and intensive living support.
Overwhelmingly, people in this part of the scheme live in group homes, with little choice over where they live, who they live with and who provides their support. Worse still, they face high rates of violence, abuse, neglect and exploitation.
Intensive housing and living support is one of the most costly parts of the NDIS, coming in at around A$15 billion in 2023–24. Although this is a small group – about 7% of all NDIS participants – total support packages for these participants make up about 37% of total scheme spend.
For this price tag, Australians with disability deserve, and taxpayers expect, quality services.
New analysis in the Grattan Institute’s latest report shows how the government can create innovative alternatives to group homes that cost the same or less money.
Create alternatives for housing and living support
There are better alternatives to group homes: these are known as individualised living arrangements. The United Kingdom, Canada, and, closer to home, Western Australia , have reformed disability housing and introduced new living arrangements which offer people greater choice and a more individualised approach.
Individualised living arrangements are integrated into the community as much as possible. They draw on a mix of supports, from formal (paid-by-the-hour support workers), to semi-formal (hosts or flatmates who receive a subsidy for their expenses), to informal (family and friends).
A host arrangement is where an adult with disability on the NDIS lives with a “host family” or “host flatmate”, who is not related to them, in the host’s home, becoming part of the household. A host might be a couple or an individual, and they provide semi-formal support while going about their everyday activities.

Unai Huizi Photography/Shutterstock
A home-share arrangement is similar: an adult with disability on the NDIS lives in their own home (owned or rented) with a flatmate who provides support. Hosts and flatmates might help with emotional support, companionship, cooking, cleaning, overnight help and other household tasks, and they receive a subsidy for their expenses.
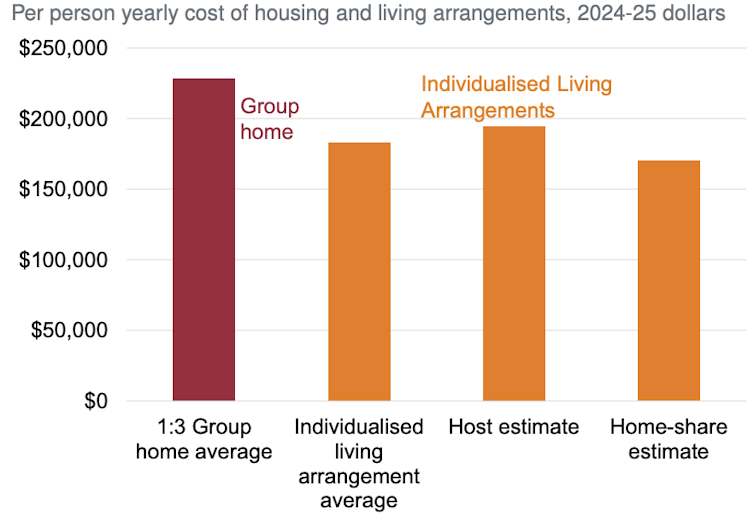
Based on our estimates, individualised living arrangements can be cheaper than group homes set at a one-to-three benchmark (one support worker for every three disabled residents), as recommended by last year’s Independent Review of the NDIS.
Individualised living arrangements cost the same or less than group
homes than the review’s proposed 1:3 benchmark
Individualised living arrangements are not only cost effective, they give people with disability choice about where they live, who they live with, and who provides their support.
Share houses, not group homes
Rather than group homes, which are run more like service facilities than people’s homes, we recommend reforms to establish share houses. So when people with disability decide to live with other people with disability and share supports, they can choose the rhythms of their daily life and who looks after them.
Moving to a system where paid support workers’ time can be shared can dramatically reduce the cost of supports, as this chart shows. This is critical in a scheme facing enormous cost pressures.
We recommend system changes too, including:
- separating housing and living supports in shared accommodation settings, as the Independent Review of the NDIS recommended
- enforceable service agreements (similar to contracts) between people with disability and providers
- support from housing and living “navigators” to establish individualised living arrangements.
- mandatory registration for providers of housing and living support, and unannounced inspections.
To give people with disability options about where they live, the government should introduce a rental payment to help people move out of their group homes and into the private rental market.
A growing feature of share houses could be sharing both formal and semi-formal support. Combining the economy of scale from sharing support workers, with semi-formal support from a housemate, would be a cost-effective way to run share houses in the future.

Marcos Castillo/Shutterstock
Time for the NDIS to get on board
Right now, people with disability have to provide copious evidence about the supports they need, and are then told what they can have and how much – often without having met the decision maker.
So people are locked into options before they’ve had a chance to try out alternatives that might be better, safer and cheaper.
Our proposal is for people with disability get a flexible budget up front. Then planning can start.
People should have access to independent advice to plan their best life within their budget. The National Disability Insurance Agency should commission housing and living navigators to give people with disability this vital help.
All of us try out different living arrangements and gradually work out what is best for us. We need information and options to choose from to get the best result – this is the same for people with disability.
Getting services right for people with the most severe disability, who need 24/7 living support should be the litmus test for any government seeking to get the NDIS back on track. Our research shows genuine choice and higher-quality services are within reach for Australians with disability – and governments don’t have to spend buckets more to get it done.
Sam Bennett, Disability Program Director, Grattan Institute and Hannah Orban, Associate Disability Program, Grattan Institute
This article is republished from The Conversation under a Creative Commons license. Read the original article.










Our most vulnerable really need the most support to independently supervise the quality of the care they receive. Perhaps the Navigators could do 3 unannounced visits to each Participant per year, just to make sure Participant are being looked after really well. That information will also help the Navigators understand which services can be relied upon for new Participants. It will need more Navigators to handle the extra work but we have surely learnt that intensive
(and expensive) NDIS support needs intensive oversight.