Caring for someone living with dementia isn’t always easy – it can be frustrating, overwhelming and even, at times, frightening.
Though every case of dementia is different, the changes that take place in a person’s brain when they have dementia can have a range of effects, including apathy, depression, sadness, anger, agitation, confusion, or even aggression.
Dementia also changes a person’s senses, their hearing, sight, taste, smell and sense of touch.
Some of the challenges you may be experiencing caring for a person living with dementia may be caused by the deterioration of their sensory system and lead to poor communication.
If we can acknowledge the changing sensory abilities of someone living with dementia, understand the level of their sensory awareness and therefore their capabilities, we are in a better position to be able to support and care for the person in a way that works with their limitations and meets their needs.
Dementia Live® is a training tool that has been developed by the AGE-u-cate Training Institute offered in Australia through BrainSparks to help carers understand what it might feel like to live with dementia.
The program immerses carers in an environment where their senses are muted, helping them understand and have a greater appreciation of what it might be like to live with dementia.
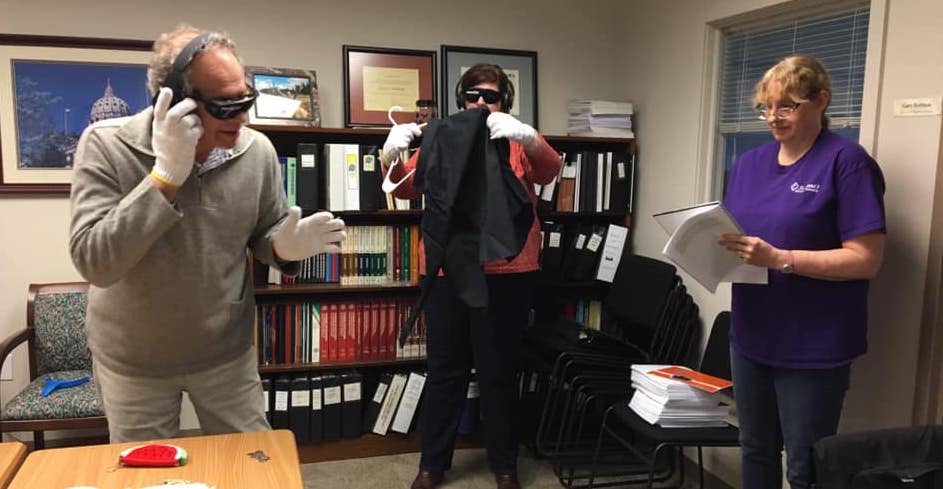
Dementia Live participants put on gear that mimics having reduced sensory abilities such as the loss of peripheral vision, tactile senses, and hearing. Following that, they are asked to complete a number of simple everyday tasks such as making a phone call or buttoning up a shirt.
With their senses compromised, the Dementia Live experience gives participants an idea of how they might feel if they lived with dementia.
Lynne Gardner is one of AGE-u-cate’s Dementia Live master trainers who teach professional carers of people living with dementia how to run the experience, as well as providing the experience for families caring for loved ones with dementia at home.
“The thing that struck me when I first did the course was, wow, this looks like it can actually teach empathy,” said Ms Gardner
“I always thought empathy was an innate ability that came from within, but when you’re doing Dementia Live, you do experience what it’s like to have sensory deficits.”
“It’s very, very difficult to do even simple, everyday tasks when you can’t feel, see or hear properly,” she said.
People who have gone through the experience say it was easy to forget what you were supposed to be doing. The emotions participants feel become evident not only to them but also to the person observing them.
They can become distracted because the tasks were made much more difficult with their senses dulled. Ms Gardener said that she lost interest in what she was doing. Some get frustrated because they can’t complete the tasks,while others describe it simply as “Wow!” as words fail them and as they begin to understand the consequences of sensory loss and therefore what it might be like to live with dementia.
What makes the experience even more powerful is the discussion after the participants have gone through the training, where they are encouraged to talk about their feelings in the empowerment session.
“Talking about it afterwards is really important,” Ms Gardener said. “The range of emotions they can experience in the short training time is absolutely extraordinary and can deliver insights into experience with clients or loved ones”. It is discussions like these that bring about transformational change.

One client of Ms Gardener,a young woman in her early 20s,had completed the course as she wanted to learn more about dementia. The young woman’s grandmother had recently been diagnosed with the condition and had moved in with her family.
After the experience, the young woman said, “Now I get it. I understand the frustration. Now I know why she gets angry. Just getting dressed is so difficult.”
The professional caregivers almost always say they will no longer rush people living with dementia.
“They say, ‘I’m never going to rush in again because I realise, yes, it’s hard, but I’m going to encourage them instead – do with, rather than do for’”, Ms Gardener said.
Carers say they have thought they were doing the right thing by rushing in and doing tasks for residents living with dementia, but the course made them realise that person might simply benefit from having more time to do what they can, in other words, use their existing abilities.
If help is required, carers say they will ask for permission, rather than just say this is what I’m going to do.
Throughout the trainings, those subtle differences keep coming up, with similar messages heard time and time again. Through Dementia Live we can get away from the stigma that people living with dementia may already feel because it takes them longer than usual to do things, or they fumble or act strangely. Rushing in to do jobs for them can only make them feel worse.
The feedback from participants once they return to work after doing the course is often around the calmness they notice and their ability to look for reasons to explain clients’ emotions.
Carers start to slow things down and take their time. They no longer rush, which means that the people they’re dealing with are calmer too.
One example of how they change their approach is they might let the person choose what they want to wear, rather than the carer choosing for them. In other words, the care recipient’s wants and needs are respected.
Dementia Live allows you to understand what it might feel like to live with dementia. That insight creates empathy and compassion, which makes it easier to look into the world of someone with dementia.
Instead of brushing off feelings as a normal part of dementia, we can look into their world and see it through their eyes. Anger, frustration, and confusion may make up some of their everyday lives and we can adopt different approaches and techniques to help them cope.
True person-centred care considers the needs of the person with dementia. Most carers understand this and the Dementia Live experience opens a new door to care.
“This person must be treated as a person. You can’t just say ‘she’s got dementia, it’s behavioural’,” Ms Gardener said. If there are symptoms that need to be addressed, then it’s up to professional caregivers to determine what that unmet need is, what has caused it, and determine how to alleviate that “as much as is humanly possible”.
The Dementia Live experience is available in a three hour event, or as one-day practitioner training for use in facilities, communities or professional practices.
You can find out more about Dementia Live by contacting Sue Silcox on 0402 319 361 or sue@brainsparks.com.au, or visit the Brainsparks website.
Image: Participants in a Dementia Live training course (image supplied).
Sue is a passionate, compassionate carer and brings light to bear on a topic that needs enlightenment. Our carers are stressed and perhaps even as distressed as those they care for. Dementia Live is a fantastic tool for family and professional carers. Thank you Sue for such a clear explanation of the program and the insights gained by participants.
Reading this as an 84 yr old female diagnosed with FTD some six months ago and noticing this happening to me insidiously I am very scared. I wish someone in my family would do this course so they “would get it” as I am conscious at this point in time, they don’t. Makes me feel very lonely, misunderstood and even patronised at times. Turning into such a misery, I hate it. Love using my iPad, so afraid the abilities I still have will be gradually wittled away and I will become a non-person.
Good afternoon, Jeanne, I have just read your comment from the Hello Care article and it makes me very sad that you are facing dementia on your own. Whereabouts do you live? And is your family near? I would certainly like to help you in any way I can, even if it is only an email or a story that will help cheer you up on a day when you are feeling low.
Although I instigated the article, it is my desire to have families, communities, aged care staff and organisations, like shops and banks, understand, to a small degree, what you live through each day. That way, we can all properly bring about change and reduce the stigma and lack of control that you feel. It is a tough job, but your email has given me resolve to keep on going with it.
Here is a link to a mini book that I recently wrote. It is on the BrainSparks website and you will be able to download it. You will need to add your name and email address but I hope that it will give you some reasons to get through each day. It is very easy to read, and maybe you can ask your family to read it. https://www.brainsparks.com.au/online-courses/#ebook
Please feel free to contact me at any time.
I have completed the Dementia Live Experience and it is a mind-opening understanding of the difficulties and limitations people living with dementia have to cope with every hour of every day. Every carer – and their manager – should experience this to bring greater understanding of and empathy for the people they care for.
Dementia Live is a great training program that helps us understand the reality for many living in the community and in care.
Lets make inclusive community for all a normal part of design thinking.