Australians must change the “ecosystem” of care to incorporate dementia to a greater degree, even if it means we have to do it ourselves, an aged care workforce expert has urged.
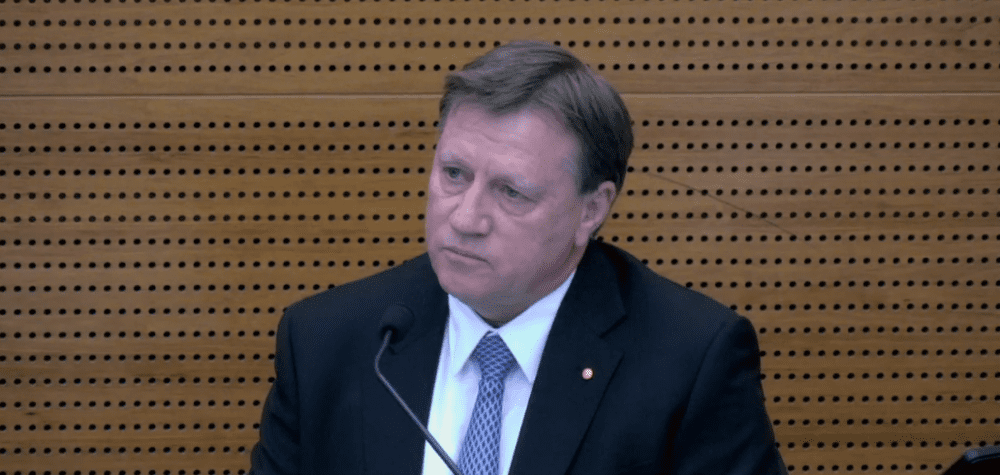
Professor John Pollaers OAM, former chair of the Australian Workforce Taskforce, said Australians who want to see improvements to the way we care for the older members of our community, including those who are living with dementia, must take some responsibility themselves for the way care is delivered.
He encouraged those listening in to Dementia Australia’s ‘National Symposium Series 2020’ to “awaken their inner activist”.
He hoped his comments would help the industry “find a way forward”, rather than “piling more pressure onto an already burdened community” in what is a “difficult time” for the sector.
“Fed up” with hearing about a “big stick” approach, Professor Pollaers said he wanted to hear about improvements that can help people “get things done”.
Professor Pollaers, whose taskforce prepared the report ‘A matter of care – Australia’s aged care workforce strategy’, said members of his generation must take matters into their own hands. The report remains unacted upon two years after it was handed to the government, the issues “kicked down the road” by the government.
“Unless we do something about it, it ain’t going to change,” he said. “The only people who are going to solve this problem are us.”
He encouraged listeners to “band together to solve the problems”, to “set a determined agenda” to address the issues that have been “hanging around for far too long”.
In a sign of just how widespread concern about dementia care is at the present moment, there were 1,100 listening on the webinar, and more than 4,000 have registered for the series.
Professor Pollaers said we already know what people want in order to deliver quality care for those who are living with dementia.
People want to hold onto their identity through their dementia journey, they want carers to be partners in delivering care, they want flexibility in the provision of care, they want those living with dementia to be able to continue to engage in meaningful activities and live in home-like settings, they want dementia-specific staff training, and they want a supportive leadership and culture.
Professor Pollaers said the ‘Matter of care’ report proposed a new ‘holistic’ model of care, with five key elements that should be included in every dementia care plan:
Personal care workers can put these elements in place, Professor Pollareas noted.
As a carer note, “It’s having the time to spend with people. Getting to know who they are, their likes and dislikes. That’s what matters.”
If the industry can get care for those living with dementia right, the care will be right for all people who are living with ageing, Professor Pollaers said.
“The time for talk is over… we know these issues have existed. Dementia has sat at the heart of the industry roadmap for a number of years, yet we haven’t seen the level of progress we need.”
When a member of the audience asked about introducing a Cert IV qualification for care workers, Professor Pollaers described the “cumbersome” nature of the training system in Australia and said providers already have the resources available to them to deliver the training they need.
Courses through Dementia Australia or the Wicking Dementia Centre are often free, flexible and readily available.
“Rolling out programs across the industry should not be difficult,” Professor Pollaers said.
“If you want to change any training package, it goes through a process review that can take up to three years to complete,” he said. “You then need to go into a teach out phase for a year, teaching the old program before the new programs are put in place.”
University programs can be developed in weeks, not years, he said.
A lot of the “richness” in Australia’s aged care training is pushed into elective subjects, which a lot of the registered training organisations don’t provide because they’re costly and they extend the length of the program, Professor Pollaers observed.
“Organisations themselves have a responsibility to put the training in place for their own teams,” he said.
He recommended a simple change in the current training requirements could be made to ensure the electives are delivered to aged care staff.
Training should be broken down into “munchable chunks” to “enable as many people in this industry as possible to get basic level training.”
“We don’t need a government system to do that,” Professor Pollaers said.
Too often, the industry looks at how to make dementia services profitable or they wait to see when the service will be delivered to them.
“The peak bodies every year spend a lot of money on webinars and conferences to entertain their membership, if that time and that money was devoted to educating people about how to operate in this environment, the key tips, the sharing of best practice, then we’d make a lot of progress.
“The key problem in this industry is we’re always waiting for somebody else to come out with the slick new program rather than saying, what are the skills that are missing, let’s make sure we nail those.”
One thing all aged care organisations can do is make sure each of their staff go through one of Dementia Australia’s 1.5 hour training modules as a necessary part of their ongoing training, as is required in the NDIS with the relevant training.
Even this little amount of training will help to increase the level of understanding in the community, Professor Pollaers said.
With 60 per cent of providers operating at a loss, a listener asked Professor Pollaers who would pay for the training.
Professor Pollaers acknowledged the industry is about 35 per cent underfunded to the tune of around $3.5 billion, but he said, “If we keep putting funding to the front of the agenda, then the things the industry can do for themselves get put to the back of the queue.
“It’s in the community’s interests and in the employee’s interest to focus on the things we can do for ourselves, while putting pressure on the government and the CEOs to lobby for those increases in funding.”
Professor Pollaers listed changes that can be made for little to no cost: dementia specific training, acknowledgement of the role of carers and families, providing meaningful activities, creating a homely environment that is focused on support, having strong feedback and complaints systems, and making sure people feel safe to provide feedback.
Despite the prevalence of dementia in the community, it is not yet core business in aged care.
Leaders need to develop a culture that supports dementia, build a workforce capacity that can support people living with dementia, and they should commit to embedding quality dementia care into their continuous improvement plans.
Five key groups have a leadership role to play, Dementia Australia, providers, the broader industry, government and the regulator. Families must also be part of the conversation.
“If boards better understood dementia and the opportunity it presents in providing better care to everyone, then, top down, they’d have a better understanding of what’s required,” Professor Pollaers said.
We need to change the “ecosystem of care” to consider the nature and role of dementia, Professor Pollaers said.
“Let’s stop reinventing the wheel. We know what people living with dementia want. We know what actions are required to improve the workforce.
“Let’s not do another of those pieces of work so we can just kick this down the road. Let’s say this is good enough for now, let’s leave things as they stand, and let’s focus on holding each of ourselves accountable, and other stakeholders, for the delivery of it.”
To find out more about Dementia Australia’s free National Symposium Series 2020, visit their website. The next symposium will be held at 11am, 18 August 2020 and will feature the Aged Care Quality and Safety Commissioner, Janet Anderson.